
Healthcare laboratory services are diverse in nature. Laboratory billing and coding is a daunting task. Healthcare providers rely on the test reports to diagnose and treat the medical illness. Thus, the diagnostic services as well as the financial stability of a healthcare facility depend on the accurate processing of laboratory billing.
According to a study by the National Library of Medicine, in the US, laboratory services are the highest level of medical activity performed annually. The gross laboratory tests cross 14 billion tests, and 70% of medical decisions depend on lab results.
This blog aims to explore the basic understanding of laboratory billing, CPT and ICD10 codes, the billing process, requirements, and different software used in laboratories.
What is laboratory billing and coding?
Laboratory billing and coding is the process of submitting claims for laboratory services. This includes blood tests, urine tests, screenings, tissue analysis, etc. Pathology tests, microbiology studies, and genetic testing also fall under laboratory services. All these tests are first translated into diagnostic CPT and procedural ICD10 codes. These codes, along with the necessary documentation, are then submitted to insurance companies for reimbursement. Medical laboratories contribute ample revenue to the total revenue of the hospital.
According to a report from Global Clinical Laboratory tests Market, the net revenue generated by the laboratory market in 2022 was US$105.8 billion. The market is expected to observe a spike up to US$ 256.3 billion by 2032. This substantial portion of revenue affects the overall financial health of the healthcare facility.
Errors in the laboratory billing process lead to claim denials or rejections. Accurate billing and coding result in timely reimbursement for laboratory services.
CPT and ICD10 Codes for Laboratory billing Services
Following is a list of important CPT and ICD codes for laboratory billing services.
| Laboratory Services | CPT Codes |
| Basic Metabolic Panel Example: Total Calcium Carbon Dioxide Potassium Sodium | 80048823108237484132 84295 |
| Complete Blood Count (CBC) Example: Automated (hematogram, WBC count, RBC count, etc.) | 85025-8502785025 |
| Blood CoagulationExample: Prothrombin time (PT) Thrombin time | 86000-860638602386038 |
| Acute Hepatitis PanelExample: Hepatitis A antibody, IgM antibody Hepatitis B surface antigen | 80074 8670987340 |
| Urinalysis ProceduresExamples: | 81000-81003 |
| Molecular Pathology Procedures | 81105-81479 |
| Therapeutic Drug Assays | 80143-80377 |
| Laboratory Services | ICD-10-CM |
| Endocrine, nutritional and metabolic diseases | E00-E89 |
| Diseases of the nervous system | G00-G99 |
| Diseases of the genitourinary system | N00-N99 |
| Neoplasms | C00-D49 |
| Diseases of the eye and adnexa | H00-H59 |
| Congenital malformations, deformations and chromosomal abnormalities | Q00-Q99 |
Laboratory Billing and Coding process
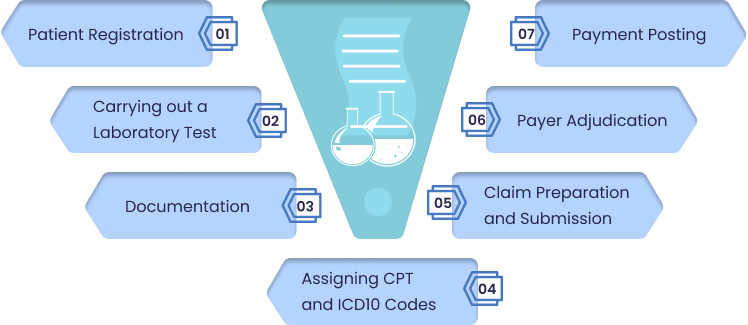
A typical laboratory billing and coding process involves several steps, as explained below:
Step 1: Patient Registration
The process starts with patient registration. All the relevant information, such as patient demographics and insurance details, is gathered. These details are entered into the healthcare provider system.
Step 2: Carrying out a Laboratory Test
Healthcare providers order the specific laboratory tests that are essential for the patient’s treatment. The tests are based on the patient’s specific condition.
Step 3: Documentation
Detailed documentation, which includes test results, patient information, and medical conditions, is essential. This helps to streamline the billing and coding processes.
Step 4: Assigning CPT and ICD10 Codes
Coders verify the documentation and assign International Classification of Diseases (ICD10) codes for patient diagnosis and Current Procedural Terminology (CPT) codes for laboratory services.
Step 5: Claim Preparation and Submission
The coded data is then used to prepare claims. These claims are submitted to the healthcare insurance company. Claims can be submitted electronically or on paper.
Step 6: Payer Adjudication
The healthcare payer now verifies every detail of the claim. If the claim is compliant with the guidelines of the insurance company, the claim is approved.
Step 7: Payment Posting
Payments are posted to the healthcare provider’s system. The process includes the total payment amount, deductibles, copayments, etc.
What are the Laboratory billing and coding requirements?
The laboratory billing and coding requirements are the set guidelines that need to be followed for accurate claim submission. Below are the major requirements that confirm timely reimbursement for healthcare providers.
Accurate and Complete Documentation
Proper and accurate documentation is the key to a clean claim submission. Healthcare providers need to maintain accurate documentation of all the laboratory services rendered to patients. This includes all types of tests, patient demographics, dates of service, etc.
Prove Medical Necessity
Healthcare providers need to submit all the necessary documents that can validate the medical necessity of laboratory services. It is the key to accurate and timely reimbursement.
Health Insurance Portability and Accountability Act (HIPAA) Compliance
Compliance with HIPAA guidelines is a must for any healthcare organization. By doing this, the patient’s privacy is safeguarded. Information is securely handled and transferred. Laboratories must follow HIPAA rules during billing and coding processes.
Adhere to National Correct Coding Initiative (NCCI) Guidelines
The National Correct Coding Initiative (NCCI) is the center for Medicare and Medicaid services. It promotes national-correct coding methodologies. Laboratories must be aware of all the guidelines and adhere to NCCI edits. This helps to prevent claim denials.
Local Coverage Determinations (LCDs) and National Coverage Determinations (NCDs)
Laboratories must understand and comply with LCDs and NCDs. They are issued by healthcare payers such as Medicare, Medicaid, etc. These documents provide rules and regulations for specific billing requirements.
Laboratory Billing Software
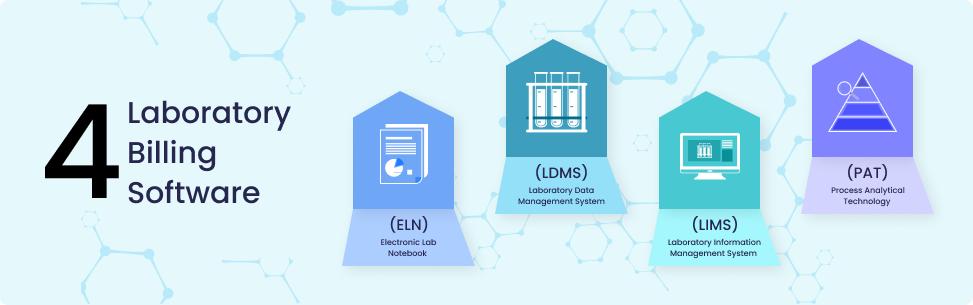
Not all the software is the right fit for every laboratory. The choice depends on the size of the laboratory and the type of tests it performs. Some of the common laboratory billing softwares are:
Electronic Lab Notebook (ELN)
An Electronic Lab Notebook (ELN) is the best replacement for paper notebooks. It is used during the R&D process. ELN has the ability to search, collaborate, and share data. It holds information about protocols, results, reports, figures, raw data, and analysis protocols.
Laboratory Information Management System (LIMS)
For routine analytical laboratories, laboratory information management systems (LIMS) are used. It is focused on samples. The software uses multiple tools that help to simplify and automate the process. The system helps with audit trails, access controls, and electronic signatures
Laboratory Data Management System (LDMS)
The Laboratory Data Management System (LDMS) acts as cloud storage for the laboratory system. Its features are audit trails, access control, electronic signatures, lifecycle management, an integrated provider portal, and collaboration.
Process Analytical Technology (PAT) Software
Process Analytical Technology (PAT) software is used for online control systems. The software accepts the analytical data and executes modifications to the production system. PAT is adaptable and custom-built.
Medheave: Your Reliable Partner in laboratory billing and coding
Medheave is a leading medical billing and coding company that excels at streamlining your revenue cycle management. The company has extended its services to hospitals, clinics, laboratories, emergency rooms, urgent care, etc. Here are several reasons why you should outsource your laboratory billing services to Medheave.
Utilization of Advanced Laboratory Billing Software
The company is utilizing advanced technology for efficient claim submission. The latest laboratory billing software ensures accurate billing and coding, clean claim submission, and timely reimbursement.
Comprehensive Coding Support
An expert team of coders is certified by the American Association of Professional Coders (AAPC) and the American Health Information Management Association (AHIMA).
The company specializes in using coding software such as Encoder Pro, CodeLink, CPC, etc., which ensures the accurate coding of laboratory services.
Compliance with the Regulatory Bodies’s Guidelines
The healthcare industry is constantly evolving. Staying updated with all the latest changes and regulatory measures is a daunting task. Medheave ensures that all the laboratory billing services are compliant with industry standards and legal requirements.
Customized Billing and Coding solutions
The company is aware of the diversity in healthcare laboratories. They are diverse in size as well as function. Medheave recognizes that each laboratory has its own unique needs. Thus, the professionals tailor solutions that cater to the specific requirements.
Wrap Up
Laboratory billing and coding play a key role in managing the overall revenue of the healthcare organization. This guideline helps to understand the basic laboratory billing processes and requirements.
Outsourcing to an expert medical billing company such as Medheave simplifies your intricate laboratory billing journey. The company ensures accuracy and efficiency in the revenue cycle. Choose Medheave as your reliable partner. Sign up today to get error-free laboratory billing services.




