According to market research analysis, the global urgent care market will surge from USD 24,624.88 million in 2022 to USD 37,222.12 million in 2030. The CAGR (Compound annual growth rate) expectation is 5.3%. This escalation in the market value depicts the explosive growth of urgent care needs among patients.
Its popularity is mainly due to the urgent medical services, which are quick, efficient, and affordable. With a boom in the market, the margin of errors in urgent care billing has also gained an upward climb. Urgent care billing mistakes result in claim denials and, hence, a loss in reimbursement.
This blog highlights all the common mistakes in urgent billing, available solutions, and how Medheave can help you with accurate urgent care billing services.
Urgent care is a healthcare service that provides immediate medical treatment for conditions that demand urgent care. It is not considered an emergency, so the patient does not visit an emergency room. These centers are equipped to handle minor injuries and infections. Urgent care billing, on the other hand, is the medical billing process for an urgent care center. It includes documentation, coding, invoicing, submitting claims, etc.
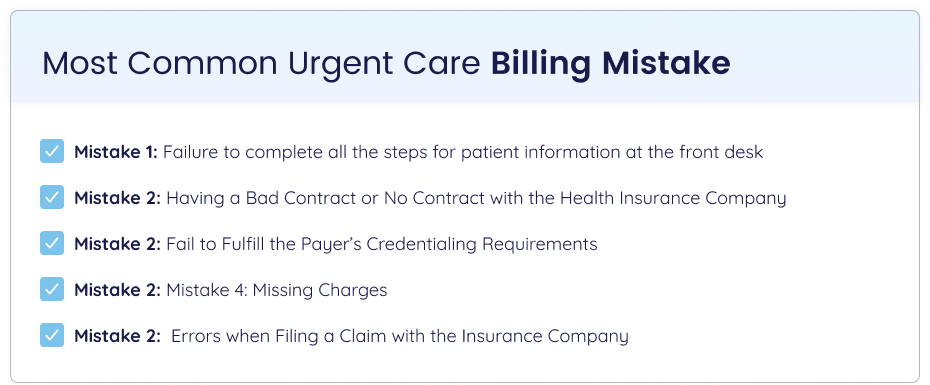
Here are the 5 most common urgent care billing mistakes, along with some available solutions.
Mistake 1: Failure to complete all the steps for patient information at the front desk
The fate of the revenue cycle is decided as soon as a patient interacts with the healthcare facility at the front desk. It is the initial point of contact and, hence, sets the table for the whole urgent care billing and coding process. Missing steps at this initial phase leads to revenue loss for the healthcare facility. The front desk can make a number of mistakes, such as
- Fails to collect comprehensive patient information.
- Failure in the patient’s insurance verification
- No clear communication about co-payment
Solution
- Make sure that the front desk collects all the required information accurately.
- Implement an effective insurance verification process to check eligibility, coverage, co-payments, etc.
- Ensure to develop clear communication to inform the patients about their financial responsibilities.
Mistake 2: Having a Bad Contract or No Contract with the Health Insurance Company
Having a contract with the healthcare payer means you have entered into a legal agreement in which the payer agrees to reimburse your healthcare facility as per the reimbursement rate set in the contract. It also enters the urgent care system as an in-network facility. Having a bad or no contract means:
- Pricing, scope, and payment terms are not properly addressed.
- The use of an ambiguous tone results in misunderstandings.
- Inadequate legal coverage puts the healthcare provider in hot water.
- There is no documented evidence of the agreement between the two entities.
Solutions
- Double-check all the required information from the patient. This ensures a fair and transparent contract between the two parties.
- Use clear language, detailing timelines, expectations,etc.
- Take help from any legal professional to minimize the legal risks.
Mistake 3: Fail to Fulfill the Payer’s Credentialing Requirements
Credentialing is the process of validating a healthcare provider’s educational background, certifications, license, professional references, and clinical experience. It helps the healthcare payer to be aware of the credibility of a healthcare provider. Not fulfilling the payer’s specific credentialing requirements results in serious repercussions for healthcare facilities. This includes:
- Not fulfilling credentialing guidelines halts the safety measures and puts the health of the patients at great risk.
- Results in legal consequences such as penalties, fines, sanctions, and even revocation of the license.
- Damages the reputation of healthcare facilities and creates trust issues.
Solutions
- Closely monitors each payer’s credentialing requirements and fulfills them.
- Ensures the implementation of regular audits and monitoring processes.
- Invest in technology, such as credentialing software, to minimize the errors in the process made by humans.
Mistake 4: Missing Charges
Missing out on valuable charges such as injections, x-rays, lab tests, and drug dosage amounts has a direct impact on the financial health of the healthcare facility. Any issue in the billing process results in claim denials and delays in reimbursement. Reasons for missing charges are:
- Providers failed to document all the services rendered to the patient.
- No proper charge-capturing process
- The staff to handle the charges at the urgent care center is not fully aware of all billable services.
- Fails to make the diagnosis code as specific as it should be.
- Forgets to add the required modifiers
Solutions
- Thorough revisions and regular sessions to evaluate the accuracy of the documentation.
- Implement an integrated system with an automated charge capture system and electronic health record (EHR).
- Regular internal audits to verify the correct usage of modifiers and diagnostic codes
- Request labs to double-check all the charges.
- Train staff about the value of charge capture and highlight the specifications for billing services.
Mistake 5: Errors when Filing a Claim with the Insurance Company
Incorrect claim filing with the insurance company results in claim denials or rejections. The reimbursement is delayed. Accuracy in all the steps involved in claim submission is essential. The most common issues with incorrect claim filing include:
- Incorrect usage of diagnostic ICD10 and procedural CPT codes.
- Missing the information related to the patient’s demographics, insurance details, etc.
- Unable to meet the submission deadlines set by the healthcare payers.
- Failed to verify the insurance eligibility prior to claim submission.
- Incomplete data on claim forms
Solutions
- Double-check all the necessary information before entering it into the billing system.
- Hire coding experts who have special knowledge about the diagnostic and procedural codes.
- Make sure that all the necessary and supporting documents are attached to the claim form.
- Set multiple reminders for claim submission deadlines. Track claim status.
Medheave medical billing experts have a team of professionals with specific knowledge about urgent care billing guidelines and new requirements. The company ensures that all the urgent care billing claims are submitted accurately. They effectively handle all the insurance verification processes for you.
The company is aligned with industry standards. They have an integrated charge-capturing system that reduces the chance of missing valuable charges. All the denials or rejections are handled by experts.
By outsourcing all of your urgent care billing, you can enjoy accuracy, efficiency, and timely reimbursement. Contact us now for a higher clean claim rate in urgent care billing.