Do you often get overburdened when dealing with gastroenterology medical billing and feel like you are solving a complex riddle while submitting each claim? It is, in fact, a familiar battleground for healthcare physicians. From juggling diagnostic codes to managing insurance requirements, the process can be complex.
Gastroenterology, as a medical specialty, covers a broad spectrum of techniques and diagnoses, each of which has its own specific coding and documentation needs. In this blog, we will shed some light on this tricky topic and give you a comprehensive guide to bill claims for GI procedures. We will go into details about things you must know, like common CPT codes used, the impact on revenue generation, challenges faced, and tips to enhance your gastroenterology practice.
Gastroenterology deals with the diagnosis and treatment of all issues related to the gastrointestinal tract. However, gastroenterology billing is the process by which gastroenterologists create charges for medical services related to the digestive tract. The billing process starts with the submission of claims for all the services rendered and ends with reimbursements received from insurance companies.
The documented information is first translated into standardized codes. These codes act as a language understandable by every entity in the healthcare industry. However, the gastroenterology billing process is not this simple. It requires attention to detail and compliance with the regulatory bodies.
The following table covers a wide range of gastroenterology practices such as colonoscopies, endoscopies, etc.
| CPT Codes | Procedures Performed in Gastroenterology Practice |
| 43235 | Esophagogastroduodenoscopy (EGD), diagnostic, including collection of specimen(s) by brushing or washing when performed, with or without biopsy(ies), with or without insertion of a tube, with or without injection of a substance; with biopsy(ies) |
| 43239 | Esophagogastroduodenoscopy (EGD), diagnostic, including collection of specimen(s) by brushing or washing when performed, with or without biopsy(ies), with or without insertion of a tube, with or without injection of a substance |
| 45380 | Colonoscopy, flexible, proximal to splenic flexure; with biopsy, single or multiple |
| 45390 | Colonoscopy, flexible, proximal to splenic flexure; with ablation of tumor(s), polyp(s), or other lesion(s) not amenable to removal by hot biopsy forceps or bipolar cautery |
| 45378 | Colonoscopy, flexible, proximal to splenic flexure; diagnostic, including collection of specimen(s) by brushing or washing, when performed |
| 45385 | Colonoscopy, flexible, proximal to splenic flexure; with removal of tumor(s), polyp(s), or other lesion(s) by hot biopsy forceps or bipolar cautery |
| 43235 | Esophagogastroduodenoscopy (EGD), diagnostic, including collection of specimen(s) by brushing or washing when performed, with or without biopsy(ies), with or without insertion of a tube, with or without injection of a substance; with biopsy(ies) |
| 43249 | Upper gastrointestinal endoscopy including esophagus, stomach, and either the duodenum and/or jejunum as appropriate; with directed placement of percutaneous gastrostomy tube |
| 43253 | Upper gastrointestinal endoscopy including esophagus, stomach, and either the duodenum and/or jejunum as appropriate; with transendoscopic balloon dilation of esophagus (less than 30 mm diameter) |
| 45391 | Colonoscopy, flexible, proximal to splenic flexure; with control of bleeding, any method |
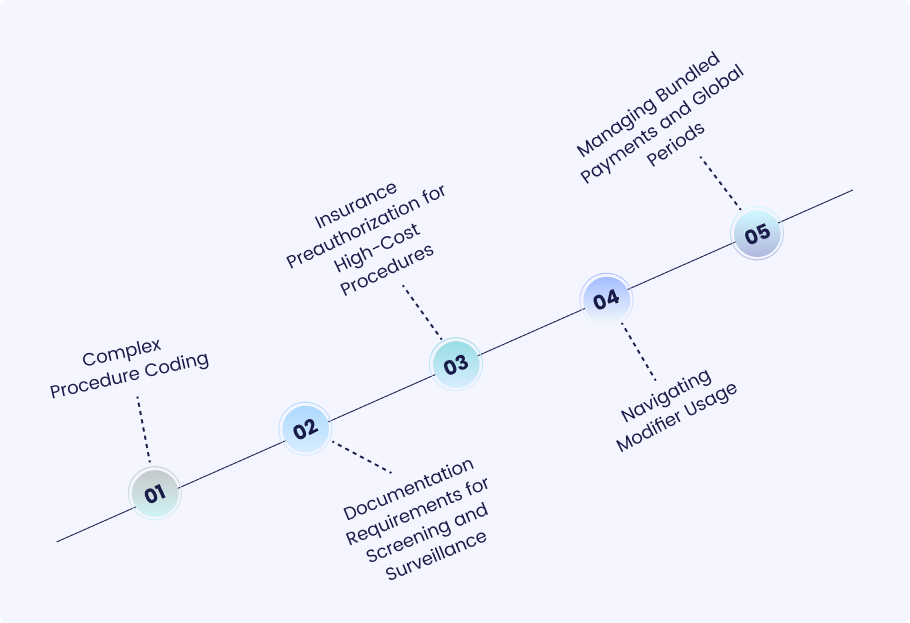
Here are some specific challenges faced by the billers due to the complex nature of the gastroenterology procedures:
Complex Procedure Coding
Gastroenterology involves complex diagnostic procedures, each of which carries specific coding rules and guidelines. Discriminating between different similar procedures and settling on the right current procedural terminology (CPT) code can be an arduous task. Accurate coding is key to correct reimbursement and compliance. Hence, it should not be underestimated.
Documentation Requirements for Screening and Surveillance
Common gastroenterology clinics perform colon cancer screening and surveillance with the help of fiber-optic endoscopes. Meeting documentation requirements becomes mandatory for these procedures. This includes documentation indications, findings, and follow-up recommendations for being on par with payer guidelines and making it possible to get reimbursement. Inadequate or insufficient documentation can result in claim denials or audits.
Insurance Preauthorization for High-Cost Procedures
Some gastroenterological interventions, such as endoscopic ultrasound (EUS) and endoscopic retrograde cholangiopancreatography (ERCP), need pre-authorization from the insurance companies. Denials of pre-authorization directly impact patient care plans. This, in turn, interrupts the financial health of the healthcare practice.
Navigating Modifier Usage
The gastroenterology procedures may require the use of modifiers in order to provide more information on the type of service. However, deciding which modifier to use and how to implement it is the toughest part. Underutilization or omission of modifiers could lead to claim rejections, inaccurate billing, and underpayment.
Managing Bundled Payments and Global Periods
Gastroenterology procedures such as bundled payments and global periods may incur a total sum that includes all related services’ fees. Maintaining invoices and reimbursements applicable to bundled payment models, as well as respecting global period guidelines, may be very complex. It is important that appropriate documentation and coding are done and the payer policies concerning bundled payments are well understood to avoid underpayment and overpayment.
Also Read: Common Medical Billing Mistakes
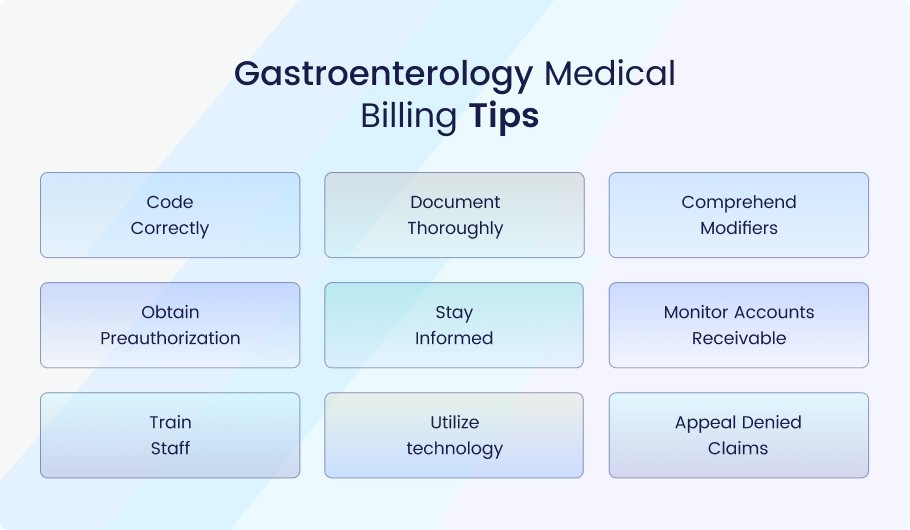
Following are some pro-tips that can effectively enhance your gastroenterology billing practice:
Code Correctly: Provide the correct confirmation for the gastroenterology procedures using appropriate CPT codes.
Document Thoroughly: Prepare clear documentation of patient visits, the services rendered, and medical necessity to substantiate bills.
Comprehend Modifiers: Utilize modifiers to convey more accurate details about the condition depicted in gastroenterology procedures.
Obtain Preauthorization: Verify insurance coverage and get pre-authorization for high-cost outlays to ensure money is not delayed by disputes and delays in reimbursement.
Stay Informed: Keep track of Medicare and Medicaid billing guidelines, payer policies, and regulatory changes that could affect the way billing is done in gastroenterology.
Monitor Accounts Receivable: Make a habit of checking the accounts receivable to locate and correct any billing mistakes, claim denials, or overdue payments swiftly and timely.
Train Staff: Implement detailed training for billing personnel on gastrointestinal billing procedures, coding criteria, and documentation requirements.
Utilize technology: Harness software and EMRs to ease billing processes, reduce errors, and enhance efficiency.
Appeal Denied Claims: Create an active plan to appeal the rejected claims with the help of comprehensive documentation as well as prompt appeals submissions.
GI billing (gastroenterology billing) plays a significant role in determining the financial health of a healthcare organization. It controls the revenue generation and its impact on overall profitability. With the complexity of endoscopy billing and the strict payment rules, accurate and efficient billing approaches matter a lot as they are directly related to income generation. Errors in coding, documentation deficiencies, claim denials, and late payments can all cause the loss of revenue and financial instability for gastroenterology practices.
On the other side, gastroenterology billing allows practices to effectively manage revolving collections, reduce claim denials, and receive reimbursement in a timely manner. Proper billing systems allow not only to ensure the financial validity of the healthcare practice but also to support physicians with the delivery of proper care for patients having digestive disorders.
Medheave is your trusted and reliable partner who understands the complex structure of gastroenterology medical billing. We have years of experience and expertise in this field. Thus, we understand the common challenges that gastroenterology practices may face. We strive to offer accurate, timely billing services that are tailor specifically to your needs.
At Medheave, we emphasize data accuracy, regulatory compliance and transparency in every aspect of our billing services. We emphasize transparency in communication and collaboration. We endeavor to work closely with your practice to explore the exact needs and requirements. From coding to documentation, claims management, and revenue cycle optimization, we’re there to assist.
Leave the worries of proper gastroenterology billing to Medheave, as we are ready to tackle it like a true professional. Contact us for Further details.