
Are you aware of the number of claims your healthcare facility submits everyday? Do you know the total number of claims denied by the insurance company? Claim denials are costly. If your clean claim ratio is less than 95%, you are definitely losing revenue. A clean claim is one that is accurately submitted to the insurance company in the first place. To maintain a high clean claim rate, it is essential to first understand the role of a clean claim in medical billing.
This blog is all you need to know about clean claims: why it is important, impact on medical billing, formula to calculate the clean claim rate, risks to the billing process, and how to increase your clean claim ratio.
What is a Clean Claim in Medical Billing?
A clean claim is defined as an accurate and clear claim submission to the insurance company for reimbursement. The claim successfully fulfills all the guidelines of the healthcare payer. Thus, no extra documentation or information is requested from the healthcare provider. No delays in payment transfer to the provider is the basic benefit of a clean claim.
A clean claim is possible if:
- The claim form has all the necessary information, such as patient demographics, insurance coverage, provider information, etc.
- The claim form is complete, with all the necessary and supporting documents attached.
- The claim is submitted within the time frame provided by the insurance company.
- The claim must follow and be in accordance with the guidelines of the insurance company.
Why is it important to file a Clean Claim Rate?
According to a report from the Medical Group Management Association, filing a clean claim rate is important as:
- Denied or rejected claims result in financial loss to the healthcare facility.
- The average cost to deal with one denial and its resubmission is $25.
- 50%–60% of denials are never appealed or resubmitted
How to Calculate Clean Claims in Medical Billing?
The clean claim rate in medical billing is easy to calculate. You can divide the total number of clear claims by the total number of claims submitted to the insurance company. Then the result is multiplied by 100 to find out the percentage of clean claim rates.
Formula
Clean Claim Rate=(Total Number of Claims/Number of Clean Claims)×100
This means if the provider submits 98 clean claims out of 100, the clean claim rate is 98%. The common benchmark set by the medical billing industry is higher than 95%. Achieving a high clean claim rate is essential for effective revenue cycle management.
What is the Impact of Clean Claim on Medical Billing?
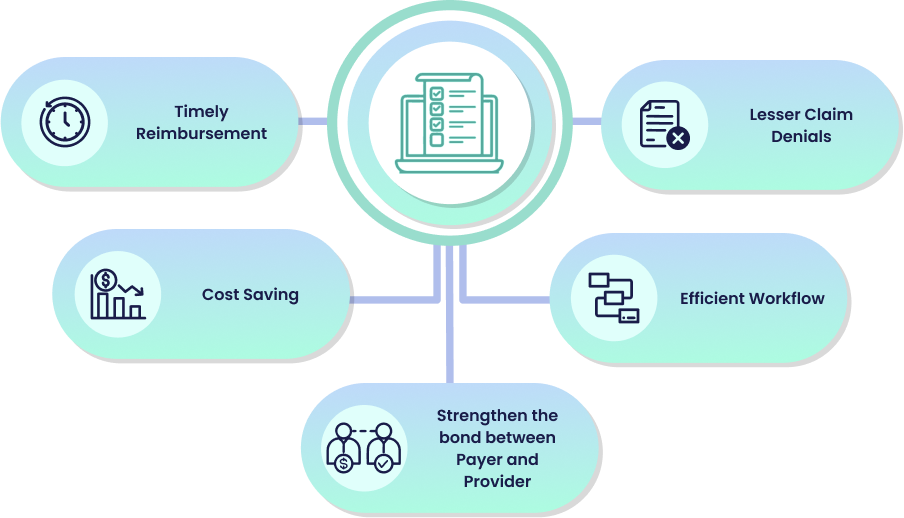
Clean claims turned out to be the major asset for any healthcare facility. It contributes to the efficiency and effectiveness of the medical billing process.
Timely Reimbursement
Clean Claims adheres to the specific guidelines of the insurance company. Thus, the company processed it quickly. This results in timely reimbursement being delivered to the healthcare provider. Clean Claim helps the provider maintain a steady cash flow for its operations.
Lesser Claim Denials
A claim that fulfills all the guidelines provided by the insurance company is less likely to be rejected or denied. If the claim is accurate and properly documented,the chances of denial are less than zero. This reduces the hassle of appeals and resubmissions.
Efficient Workflow
Clean claims help streamline the medical billing process. Providers don’t need to communicate with insurance companies about the denials. There is no need to provide extra documents to support the claim. This allows the provider to focus on patient care and increases the efficiency of the workflow.
Cost Saving
Clean claims reduce the administrative cost of the healthcare facility. No extra staff, and resources are required to deal with denials, appeals, and resubmissions of the claims.
Strengthen the bond between Payer and Provider
Clean claim submission helps foster the bond between healthcare payer and provider. Thus, there is no reason for argument. It creates a smoother interaction between the two and helps to improve patient care.
How to increase your Clean Claim Ratio?
Claim Scrubbing before Submission
Claim scrubbing acts as a checkpoint to resolve any errors present in the claim. It’s a proactive step to review the claims for any errors or compliance issues. Denials occur mostly due to coding errors or late submissions to the insurance company. Scrubbing makes sure that there is no coding error and patient information is complete and accurate.The claim is in accordance with the guidelines provided by the regulatory bodies.
Clear Communication Channel
A clear communication channel between healthcare payer, patient, and provider reduces the hassle and misunderstandings between the entities. Any information related to the billing process or queries smoothly travels and is answered.Clear communication means everyone can easily talk to each other and can resolve potential issues before claim submission.
Utilize advanced technology and Automation
Utilization of advanced technology and automation tools helps to streamline the billing process. Thus, reduces the margin of error in the claims. Claim scrubbing software can automatically detect errors before the claim submission. Insurance companies would have no chance to deny or reject the claim. By doing this, providers can only focus on patient care. He need not to worry about the paperwork, documentation, medical records, etc.

Claims that have errors in it are denied or rejected by the insurance company.This results in several risks associated with the overall efficiency of the medical billing process. Key risks include operational, financial, and regulatory implications for revenue cycle management. Risks include:
Delayed Reimbursement
Claims that are not accurate and clear require extra clarification. Healthcare providers need to provide supported documents. This directly halts the reimbursement process, as the insurance company takes longer to deal with these kinds of claims.
Increased Administrative Costs
In order to resolve the issue of claim denials and rejections, additional staff is required to find out the denial reasons, appeal, and resubmit the claims. This increases the labor costs for the healthcare facility.
Compliance Issue
Compliance issues with the healthcare payer arise when the provider submits incomplete claims with errors in them. This can result in penalties, fines, or legal action against the provider.
Patient Dissatisfaction
Any error during claim submission results in the patient’s receiving incorrect billing. This slows the claim processing speed, leading to dissatisfaction among patients. They stop trusting their healthcare provider.-
Redirection of Resources
Resources such as healthcare staff and financial assets are diverted from other essential tasks to address the denied claims. This puts a question mark on the efficiency and productivity of healthcare facilities.
Improve your Clean Claims Ratios with Medheave
Outsourcing your billing process to a medical billing company like Medheave is a successful move to enhance your clean claim rate. Medheave has a proven record of 98% clean claim rate on first submission. The company has an expert team dedicated to maintaining error-free claim submissions. This not only reduces the denial rate but also improves the overall efficiency of revenue cycle management. By outsourcing to Medheave, one can enjoy a range of advantages, such as efficiency, expertise, cost-effectiveness, and the ability to focus on patient care. Contact us today for an error-free, clean claim submission.




