
A patient visits the hospital and receives medical care. A parallel process also takes place called hospital billing, which is a far more complex and confusing job for hospital staff. The medical record of the patient is first translated into standardized codes. These codes are then billed to the insurance company for reimbursement. It sounds simple, but it is not. Welcome to the world of hospital medical billing service. This blog will help you define the path from patient care to medical billing.
What is Hospital Billing?
Hospital billing, also known as institutional billing, is the process of the submission of the claims for in-patient and out-patient services provided by the hospital and receiving reimbursement from the insurance company. It is far more complex than professional billing as it includes bills for laboratory services, medical supplies and equipment, radiology, etc.
Difference between Hospital billing and Physician Billing
| Hospital Billing | Physician Billing |
| Hospital billing is far more complex as it covers a wide range of services. | Physician billing is less complex as it covers the services of only a single provider. |
| It covers the billing process only. | It covers both the billing and coding processes. |
| The UB-04 form is used for case filing. It is white in color with red letters on it. | The CMS-1500 form is used for case charging. It is white in color with red alphabets. |
| The electronic version of UB-04 is 837-I. | The electronic version of CMS-1500 is 837-P. |
| The risk of denied claims is higher for hospital billing due to the complexity of the process. | The risk of denial claims is much lower than hospital billing. |
How does Hospital Billing work?
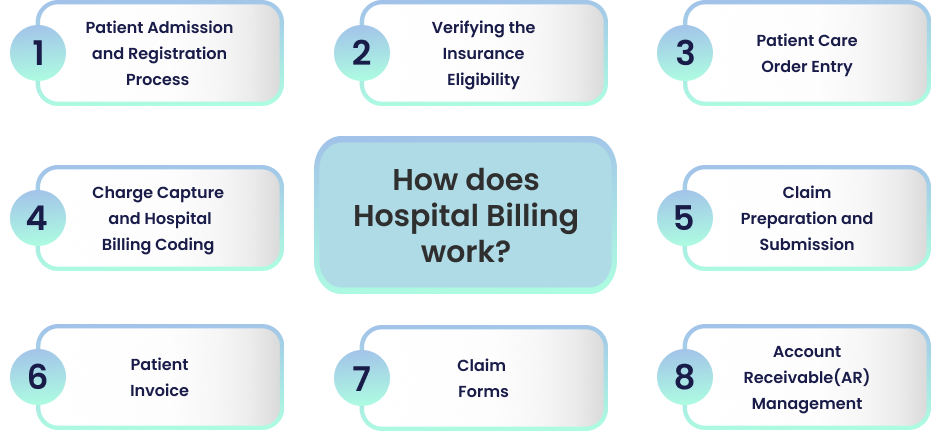
Patient Admission and Registration Process
The process of admission for inpatients and outpatients starts when the patient visits the hospital. On arrival, the patient is subjected to providing demographic information such as name, DOB, consent for treatment, and insurance policy coverage. This medical record sets the foundation of the billing process. The biller must be attentive at this point, as any error during data collection directly impacts the reimbursement process.
Verifying the Insurance Eligibility
The second most important step is the verification of patients’ eligibility for insurance company policy coverage. The hospital staff double-checks the services that can be rendered to the patient. Healthcare services are provided according to the insurance coverage of the patients. Insurance information can change at any time, so hospital billers must follow it closely and ask the patients about documentation and if the insurance information has changed. This sets the basis for accurate claim submission.
Patient Care Order Entry
At the hospital, the provider is the one who takes charge of everything. Services provided to the patient are according to the orders given by the provider. The orders are fetched into the hospital information system, which is then transferred to the related departments. The staff of various departments work together to provide services to the patient.
The supportive departments, such as radiology, laboratory, pathology, rehab, etc., provide extra services such as therapeutic and diagnostic. All the services are recorded in the medical record of the patient, which is further transcribed and documented.
Charge Capture and Hospital Billing Coding
Another crucial step in hospital billing is the charge capture and coding of medical services. Departments who provide services post the charges to the patient account through Chargemaster. All other supportive services such as pharmacies that supply the medicines, also post charges. The charge master makes a list of the services, such as diagnosis, procedures, drugs,and treatment, that the hospital provides.
The Patient Financial Service (PFS) Department converted the medical record into accurate documents. A standardized language of codes such as ICD10 and CPT is used to represent the documented information. A computer program called Encoder is utilized to assist the coding process. This translation of complex healthcare data from the hospital into a standardized format makes it easy to decode.
Claim Preparation and Submission
Hospitals compile all the coded data to generate the claims. These claims outline all the services provided to the patient in the hospital. The associated cost for each service is also mentioned. The claim is then submitted to the insurance company, following all the protocols and guidelines given by healthcare payers for timely reimbursement. Patient invoices are used to submit charges to the patient, whereas claim forms are used to submit claims to the insurance company.
Patient Invoice
It is a document prepared by the hospital and sent to the patient for the outstanding balance. It provides account activity such as the current balance and previous balance.
Claim Forms
A standard claim form, UB-92, is used to submit the claim charges to the insurance company. It is white in color with red letters on it. These forms can be printed manually and sent to the insurance company by fax. An electronic version (837-I) submits the form electronically.
Account Receivable(AR) Management
Accounts receivable (AR) management is the key to timely reimbursement. Through AR, hospitals manage and follow up on the outstanding balance. A PFS Department, commonly known as Credit and Collection, is responsible for the smooth functioning of Accounts Receivable Management. Accounts are categorised according to age, payer type, and amount due.
Wrap Up
Every detail matters in hospital billing. The purpose of the process is to provide reimbursement for the services and items rendered to the patient in a hospital. Understanding and managing these complex steps of the billing procedure is crucial for the hospital staff. A team of billing and coding professionals is required who have an understanding of hospital billing.
Medheave is a company of professional billers and coders who can handle the process in the most effective manner. Consider outsourcing your hospital billing to Medheave. Contact us today for a seamless revenue process.




