Billing has its own complications, and even for a simple procedure like tick removal, practice can shoot up if the coding part is not done right. From the accurate coding of diagnosis to claims submission, health care providers have to undergo a complex process of insurance requirements and coding regulations to obtain their payment. To the health care providers, it is important to know the proper codes to be used and all the best procedures that can go a long way in ensuring that they manage the entire billing process appropriately.
In this blog, we’ll break down everything you need to know about tick removal billing and coding, offering the billing process and the best practices to help your practice streamline the process and boost your bottom line. Whether you handle billing in-house or outsource it, understanding these key elements can make all the difference.
When coding for tick bites and removal, accurate coding depends on the patient’s condition at the time of the visit, the location of the bite, and any resulting complications. Here are some of the most relevant ICD-10 codes used to identify the diagnosis of tick removal:
ICD-10 Code for Tick Bite
- W57.XXXA – “Bitten or stung by nonvenomous insects and other nonvenomous arthropods, initial encounter.”
- This code is valid for the first time for tick bites and should be used if there is no infection or any complication related to removing the tick.
ICD-10 Codes for Tick-Related Infections
If the patient is infected or any illness that has resulted from the tick bite, then there should be other codes that accompany the diagnosis. Common complications from tick bites include:
- A69.20 – “Lyme disease, unspecified.”
- A69.21 – “Meningitis due to Lyme disease.”
- A68.9 – “Relapsing fever, unspecified.”
- B87.81 – “Loiasis, tick-borne.”
ICD-10 Code for Localized Infection from Tick Bite
If the patient has developed a localized infection at the site of the tick bite, use:
- L08.9 – “Local infection of the skin and subcutaneous tissue, unspecified.”
ICD-10 Code for Encounter for Tick Removal
In some cases, providers may use an encounter code specifically for the procedure. For follow-up or subsequent encounters:
- Z48.89 – “Encounter for other specified aftercare.”
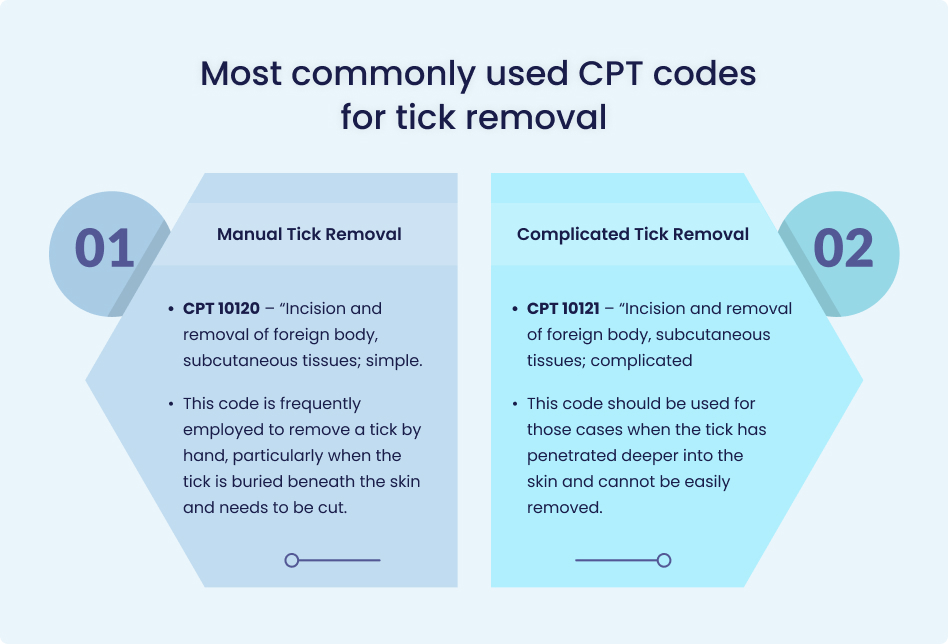
Selecting the most appropriate CPT code when billing for tick removal is critical. The correct code depends on the method used to remove the tick, whether by scraping it off or by surgery. The most commonly used CPT codes for tick removal include:
Manual Tick Removal
- CPT 10120 – “Incision and removal of foreign body, subcutaneous tissues; simple.”
- This code is frequently employed to remove a tick by hand, particularly when the tick is buried beneath the skin and needs to be cut.
Complicated Tick Removal
- CPT 10121 – “Incision and removal of foreign body, subcutaneous tissues; complicated.”
- This code should be used for those cases when the tick has penetrated deeper into the skin and cannot be easily removed.
Common and essential elements of the billing process for tick removal include, but are not limited to, the following:
Patient Encounter and Diagnosis
- Assessment: The provider examines the patient and records the tick bite as an identifying mark and decides if it has led to infections or not.
- Diagnosis: The healthcare provider identifies the specific circumstances of the case to assign the correct ICD-10 diagnosis code.
- For a simple tick bite: W57.XXXA (Bitten by a nonvenomous arthropod).
- For complications like Lyme disease or localized infections, other specific ICD-10 codes (e.g., A69.20 for Lyme disease) should be used.
Document the Procedure
- Detailed Notes: The provider should also record specific information about the tick removal process, where the tick was found, whether it was deeply embedded and how it was removed, manually or surgically.
- Follow-up Care: If more attention like infection follow up is needed then this should be well noted.
CPT Code Selection
- Determine Procedure Complexity: The provider decides which of the CPT codes corresponds to the tick removal process depending on the level of intensity.
- CPT 10120: Incision and removal of a foreign body (simple removal).
- CPT 10121: Incision and removal of a foreign body (complicated removal).
- Modifier Codes (if applicable): If this procedure is done in conjunction with other procedures, a modifier (-25: additional service during the same session) may have to be added to the code.
Verify Patient Insurance and Coverage
- Check Insurance Coverage: Check the patient’s insurance coverage so as to confirm if the tick removal process is included.
- Pre-Authorization (if needed): Insurance companies may need prior approval for elaborate interventions like excision, particularly if the diagnostic tests are conducted in a bid to identify other tick-borne illnesses.
Submit the Claim
- Complete the Claim: Complete the claim electronically and send it to the patient’s insurance company, enclosing all ICD-10 and CPT codes and modifiers.
- Include Necessary Documentation: Enclose the provider’s record or any documentation that would back up the claim to the tick removal procedure and any adverse effects experienced.
Monitor Claim Status
- Track Claim: After filing the claim, one should track it to check for any denials of the claim or requests for any more information.
- Correct Errors: If the claim has been rejected or postponed due to missing information, then correct the mistakes and submit the case again.
Receive Payment and Apply Adjustments
- Review Payment: Once the insurance company approves the claim, review the EOB to ensure the payment is correct.
- Patient Billing (if applicable): If the patient has any out-of-pocket costs (such as deductibles or coinsurance), send the patient a bill for the remaining amount.
Address Denials or Rejections
- Appeal or Resubmit Claims:If the claim has been denied, rejected, or paid less, read the EOB to understand why it was acted upon in this way and appeal or resend the claim with the correct details.
Follow-up for Additional Care
- Manage Follow-up Visits: If the patient needs a follow-up visit due to some complication, such as infection or Lyme disease diagnosis, then the claims for such visits should include diagnosis and process codes.
The proper billing for the removal of ticks is very important to avoid delays in the reimbursement process or rejection of the claims. By following the best practices, healthcare providers can streamline the billing process and maximize revenue.
Thorough Documentation
When completing the paperwork on the tick exposure, be sure to outline the location of the bite, the severity of the tick bite, and the removal technique that was used in order to maximize reimbursement. Make sure and record all the symptoms or complications if there are any so that they will not be omitted.
Correct ICD-10 and CPT Code Selection
Choose the correct ICD-10 diagnosis codes and CPT procedure codes. Wound codes such as W57.XXXA can be reported for tick bites, while for the removal of the tick, the codes CPT 10120 or 10121 should be used depending on the degree of complexity of the case.
Use Modifiers Appropriately
When tick removal is performed along with other services, add modifiers like -25 to distinguish the procedures and receive separate payment for each service.
Verify Insurance Coverage and Pre-Authorization
Review the patient’s insurance policy and find out whether prior approval is needed, especially if the tick is hard to remove or if the patient wants additional tests to be administered for tick-borne illnesses.
Conclusion
In conclusion, consideration of billing for tick removal calls for concise documentation of services, proper coding, and submission of the claim in order to quantify the right amount of reimbursement. Adherence to these best practices reduces claims error and denials making the billing process for healthcare service providers efficient. However, the flexibility involved in procuring, organizing, and monitoring charges can make billing tasks challenging, particularly when dealing with complex cases or companies that require interaction with insurance companies. If you outsource your medical billing to MedHeave Medical Billing Services, you will experience less work pressure, improve your claim filing, and dedicate more time to patient care, all while knowing that we are managing your revenue cycle.
Contact us for further details.