Managing a pain treatment center requires a great deal of effort. You and your team must join efforts to remove patient’s suffering and improve their quality of life. However, the financial health of the medical practice also matters very much to ensure its sustainability and your ability to keep on offering quality medical care.
The claim denial is certainly one of the most probable dangers to your healthcare facility’s financial stability. These denials by the health insurance payers create a serious problem with revenue cycle management (RCM). A rejected claim goes for a later or no payment, which makes it harder for you to spend on the development of new technology, hiring skilled staff, and providing the best services to your patients.
In this blog, we’ll go deeper into the issue of pain management claim denials and will provide you with the strategies to avoid these denials in your healthcare practice.
One of the major obstacles to pain management practices is the denial of claims, which affects the financial situation and increases administrative work. According to a MGMA Stat poll 2021, 83% of the healthcare providers have reported an immense increase in the claim denials. This revenue loss is estimated at an average $2,250 per denied claim. However, fear not! Here’s your arsenal of strategies to combat these revenue drainers, specifically tailored to your practice:
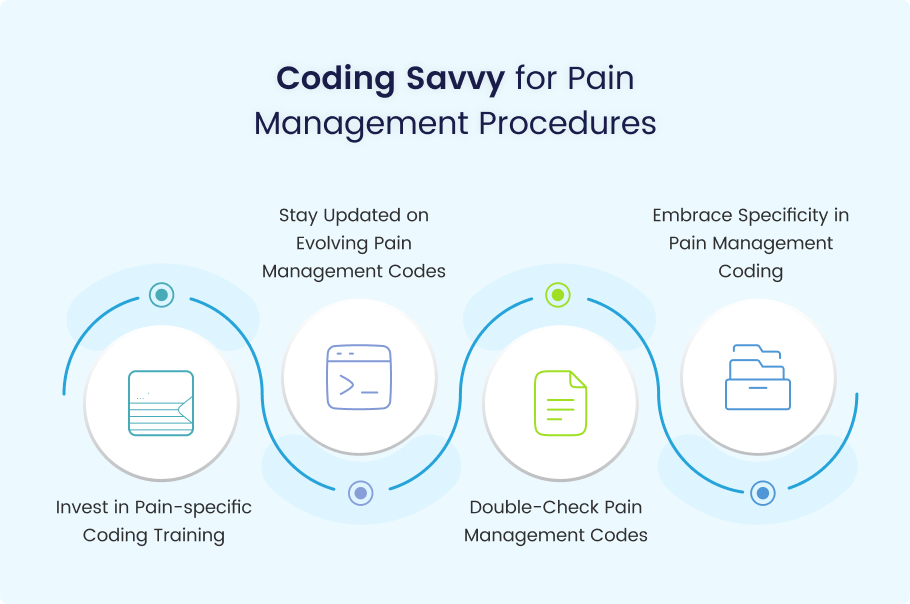
For pain management practices, accurate coding is the key to a clean claim rate. Healthcare professionals can cope with this issue through multiple strategies, such as:
Invest in Pain-specific Coding Training
Basic knowledge of general medical coding is a significant tool for healthy claim submission. That’s why it is important to train staff in the best traditions. Allocate funds to training programs and career certification programs that will address the CPT codes utilized in pain management. CPC certification is one of such certifications to ensure your team is well versed in the fine details of chronic pain codes, including injections, nerve blocks, and spinal cord stimulation procedures.
Stay Updated on Evolving Pain Management Codes
Every day, we see new medical technology, updates to existing procedures, and changes in disease classification. Get subscriptions to the AAPM and the AMA for a rundown of the existing CPT codes for pain management with the most recent updates. This will correctly guide you to the use of the most precise codes for new and emerging pain management techniques.
Double-Check Pain Management Codes
Establish a stringent verification system to scrutinize all pain management procedure codes before sending claim submissions. Apply coding software with in-built error-checking features, concentrating on pain management. Think about hiring an experienced specialist in pain management who would put the focus on error-finding.
Embrace Specificity in Pain Management Coding
It is a time-killing activity to look through pre-set codes. Make sure that you use specific CPT codes that precisely correspond to the specific type and range of pain management procedures performed. Examples include a replacement of the infertile “injection code” by the trained technical terms for facet joint injection or lumbar trigger point injection.
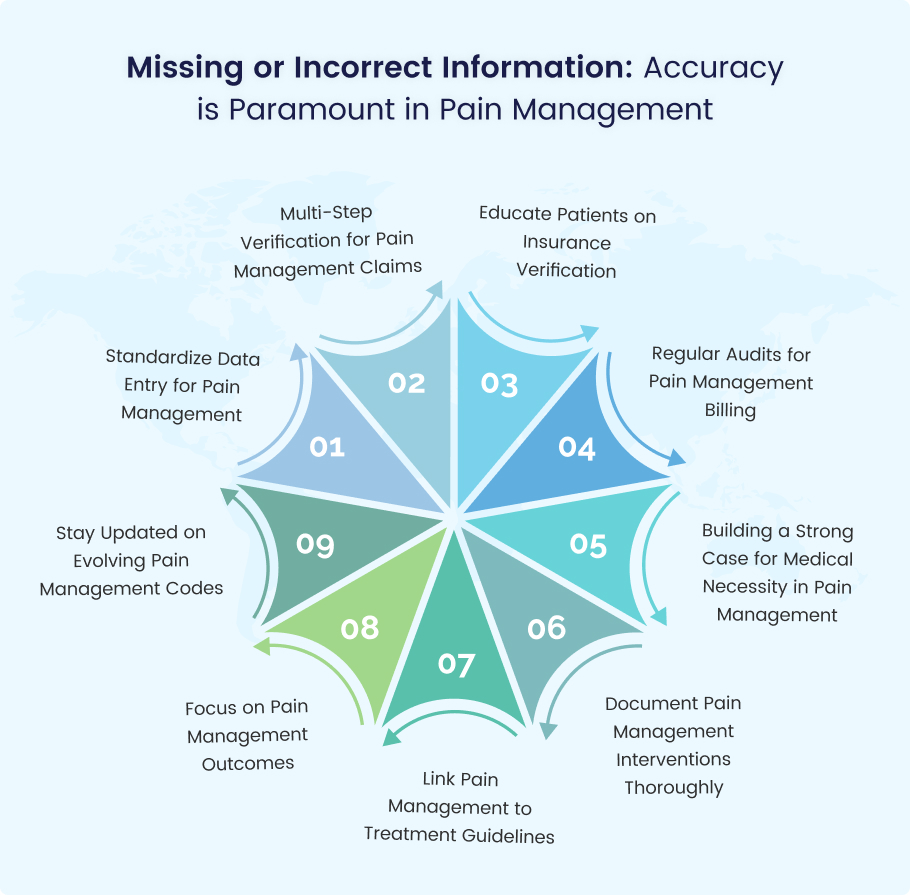
A lack or inaccuracy in the provided claim is a great flag for payers. Financial magazine Medical Economics reveals that 25% of denials can be massively attributed to the patient’s underlying information, such as demographic data, insurance coverage, and even the correct operation codes. Here’s how to ensure accuracy in your pain management practice:
Standardize Data Entry for Pain Management
Build a standard data entry technique of its own kind connected to the pain management procedures. Apply EHRs (electronic health records) with built-in fields and ‘drop-down’ menus to gain easy access to commonly used pain management diagnostics, operations, and medications. It eliminates mistakes and accounts for the right consistency of data.
Multi-Step Verification for Pain Management Claims
Develop a multistep verification system that verifies patient details, insurance information, and coding related to pain management procedures before finalizing claims. An employee should take a look at the documentation or the EHR software with pre-built reminders.
Educate Patients on Insurance Verification
Ask the patients to clarify their insurance details with you prior to an appointment or treatment. This prevents any misunderstandings on the part of the payer regarding pain management procedures from the very beginning. Thus, avoids denied claims in the future.
Regular Audits for Pain Management Billing
Conduct frequent audits of your billing system, paying special attention to the claims of pain management. Find out the normal data entry mistakes associated with pain management procedures and apply corrective measures. This assures that the payer receives every detail of every claim submitted.
Building a Strong Case for Medical Necessity in Pain Management
Proving medical necessity is a must to win the pain management claim. With no correct medical documentation indicating the procedure itself to be necessary, the claim denial rate can rise to as high as 18%. Here’s how pain management providers can fight back:
Document Pain Management Interventions Thoroughly
Preparation of thorough documents is key. Ensure that the patient’s past pain, objective physical examination results, diagnosis, and justification for the procedure selected (e.g., facet joint injection for chronic low back pain) are clearly mentioned.
Link Pain Management to Treatment Guidelines
Provide referencing to clinical guidelines and standard pain management treatment modalities by ASIPP (American Society of Interventional Pain Physicians) and AAPM (American Academy of Pain Medicine), which were developed for the pain management procedure that was done on the patient.
Focus on Pain Management Outcomes
Do not just document the procedure step by step; state the desired outcomes of pain management treatment and how improved quality of life and function will be achieved. This could involve a decrease in pain score, improved capability to perform the activities of daily living, or withdrawal of pain medication.
Consider Scribes or Dictation Software for Pain Management Documentation
Scribes or dictation software can interchangeably be valuable assets in this case. It will permit pain management providers to treat patients as individuals and provide them with the assistance they need to minimize their suffering.
Bottom Line
Claim denials should never be a perennial headache in your pain management practice. Applying the strategies presented in this blog will probably bring a lot of savings, and the flow of income will not be broken as well. It is vital to note that precise coding and flawless documentation are the fundamental pillars. Besides, adapting a proactive authorization-preparation approach is essential. Commitment to staying updated can be achieved through learning the most recent coding and billing pain management guidelines. Equipped with this arsenal of tools, you can devote yourself to the most important thing: offering the best pain management options and improving your patients’ living standards.
These strategies are robust, but if you want to save money and outsource your billing, Medheave is the choice. They dominate pain management billing, providing the healthcare providers with the skills of coding improvement, denial reduction, and efficiency improvement, which are meant to reduce costs by reducing the number of denials. Considering outsourcing, it may become a real power tool for your pain management unit. Try not to forget that financial strength is necessary for providing high-quality pain care to patients. Contact us today for further details.