Medical coding modifiers, which are alphanumeric characters, are added to HCPCS (Healthcare Common Procedure Coding System) or CPT (Current Procedural Terminology) codes. These modifiers in medical billing are used to provide additional information related to medical procedures, services, or supplies without changing the original meaning of the code. Additionally, they serve to clarify specific aspects of the provided healthcare services, ensuring accurate documentation and reimbursement. Thus, healthcare providers, billers, and medical coders need to understand the analogy of each modifier in detail.
In this blog, you will specifically explore three commonly used modifiers: 59, 25, and 91. When to use them, their importance, examples, and mistakes to avoid are all collectively discussed.
What is Modifier 59?
Modifier 59 functions as an independent code in medical billing, distinguishing a procedure or service from others conducted on the same day. It also signifies that two different procedures occur on separate parts of the body during a single visit.
When do healthcare providers use Modifier 59?
Healthcare providers use Modifier 59 when they perform multiple procedures during a single encounter, and each service or procedure is distinct and requires separate billing. It is also employed when the two services occur within a 15-minute interval.
Why is Modifier 59 important?
Modifier 59 is crucial for the medical billing process. It ensures that healthcare providers document and reimburse each procedure or service separately. Thus, it avoids confusion and potential denials.
Examples of Modifier 59
Different Anatomical Sites: If a patient receives two injections in different muscles on the same visit, healthcare providers may use Modifier 59 to indicate that they administered each injection as a separate service from the other.
Different Sessions: When the patient is undergoing therapy and treatment sessions, which are unrelated, Modifier 59 is the way to separate them.
Separate Incisions or Lesions: The surgeon may remove multiple lesions or perform separate incisions during one procedure. Modifier 59 helps to clarify that each action was required.
Here are some errors that need to be avoided when dealing with modifier 59:
Overuse
Mistake: A medical coder uses modifier 59 in excess, even when other modifiers are more specific.
Solution: Ensure that Modifier 59 is only used when none of the other suitable modifiers in medical billing accurately describe the distinctiveness of the procedure.
Unbundling Services
Mistake: breaking down bundled procedures into separate components or services without any reason.
Solution: Understand which procedures are bundled together. Use Modifier 59 only when distinct services are truly performed.
Lack of Documentation
Mistake: Lack of appropriate paperwork to substantiate the use of Modifier 59 (separate procedure) code.
Solution: Make sure the medical records clearly address why and how each ICD or procedure is justified and differentiated from the alternative.
What is Modifier 25?
In medical billing, healthcare providers use Modifier 25 to indicate that they have conducted a crucial, separately identifiable evaluation and management (E/M) encounter on the same day as another service or procedure.
When do healthcare providers use Modifier 25?
Modifier 25 is used when the patient’s visit includes both a medical procedure or service and an E/M service, which a healthcare provider can separately identify, such as an office visit. It serves to distinguish the additional assessment and management that are part of the same visit.
What is the importance of Modifier 25?
Using modifier 25 appropriately is the key to a successful billing procedure.This is helpful because it ensures that physicians receive reimbursement for the additional services involved in assessing and managing the medical condition of the patient in one visit.
Examples of Modifier 25
Routine Office Visit with Vaccination: When a patient visits the hospital for a routine checkup and receives a vaccination during that visit, healthcare providers use Modifier 25 to signify that they are separately assessing and managing the patient’s overall healthcare.
Minor Surgical Procedure with Evaluation: If a patient undergoes a minor surgical procedure, such as wart removal, and separately experiences an evaluation for an unrelated condition in the same visit, Modifier 25 distinguishes these services apart.
Follow-up Visit with Diagnostic Test: A follow-up visit, for example, when a patient comes in to discuss test results performed earlier, may also utilize Modifier 25 in order to capture additional evaluation and management of a patient’s condition.
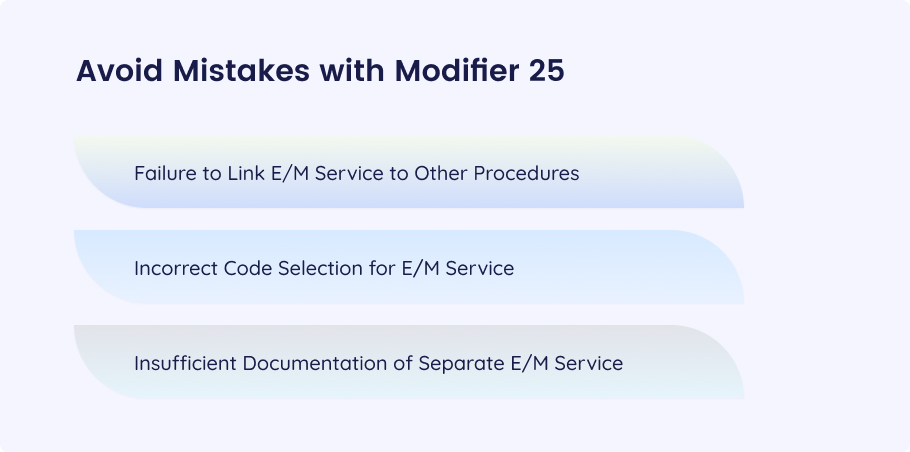
Failure to Link E/M Service to Other Procedures
Mistake: Not providing a strong nexus between the E/M service and the other procedure performed during the same encounter. Thus, it results in missed ways of appropriately billing the service.
Solution: Establish the link between the E/M service and the services and other procedures specifically. Highlight the role of the service in the maintenance of the patient’s condition.
Incorrect Code Selection for E/M Service
Mistake: Assigning an E/M code that does not closely match the characteristics of the additional E/M service, therefore coding errors.
Solution: Identify the E/M code that suitably matches the level of complexity of performing the evaluation and management work. Additionally, make sure that the selected CPT code of the separate E/M service matches the corresponding documentation.
Insufficient Documentation of Separate E/M Service
Mistake: The coding you are doing is unclear. So there is no confirmation on the actual necessity for Modifier 25.
Solution: Provide complete documentation of the individual E/M services. This includes the main issues to be addressed, like the condition, history, examination, and decision-making procedure.
What is Modifier 91?
Modifier 91 plays a vital role in laboratory billing services. Healthcare providers use it when repeating a laboratory test on the same day to obtain multiple test results.
When do healthcare providers use Modifier 59?
Modifier 91 is used when the physician repeats the same laboratory test multiple times to confirm the test results on the same day.
What is the importance of Modifier 91?
Modifier 91 indicates that the healthcare provider repeats a specific laboratory test multiple times. By using the 91 modifier, healthcare providers reduce the chances of errors and ensure they receive proper reimbursement for the additional work performed at the lab.
Examples of Modifier 91
Blood Tests: If a patient goes through several tests for the monitoring of different aspects of his health, including the glucose level and cholesterol level, then she or he will use the modifier 91 to indicate the repetitive nature of the tests.
Diagnostic Imaging: If a patient requires several x-rays or scans in a single day to track the progression of a disease or ensure the precision of results, we will apply Modifier 91 to every subsequent procedure code.
Electrocardiograms (ECGs): ECGs are performed on a patient several times during the day to monitor changes in the activity of or the patient’s response to treatment. Modifier 91 is appended to the ECG procedure codes for the repeated tests.
Urinalysis: When conducting several urinalysis tests within a single day to track kidney function or detect abnormalities, healthcare providers utilize Modifier 91 on the claim form to denote the repetition of the tests.
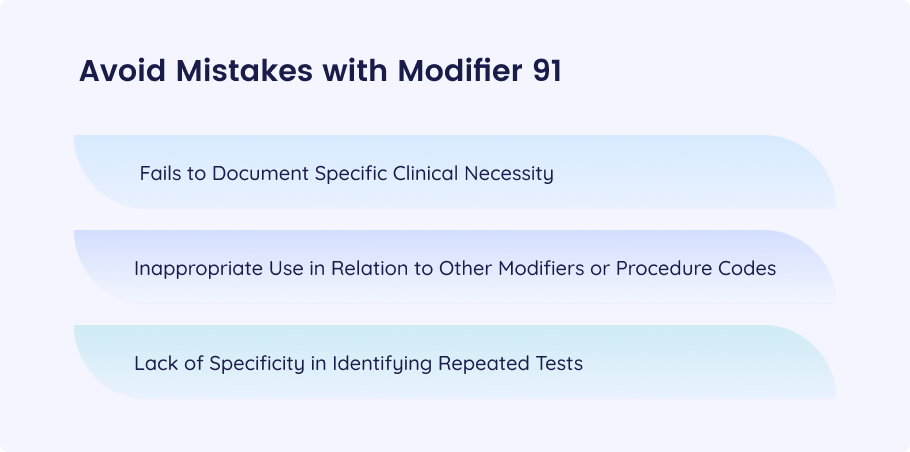
Fails to Document Specific Clinical Necessity
Mistake: Reporting laboratory test repetitions without the exact reason for the lab requests and the need for additional results.
Solution: Seek documentation that clearly shows the reasons for repeat testing and also pinpoints how the patient’s decisions are influenced.
Inappropriate Use in Relation to Other Modifiers or Procedure Codes
Mistake: Inappropriate use of Modifier 91 in relation to other modifiers and procedure codes causes billing discrepancies.
Solution: Ensure accurate placement of modifier 91 in the context of other modifiers and procedure codes, strictly following coding guidelines and billing guidelines.
Lack of Specificity in Identifying Repeated Tests
Mistake: Fails to clearly highlight the necessity of repeating laboratory tests. This makes it difficult for healthcare insurance companies to establish the requirement for additional testing.
Solution: List the specific tests that were repeatedly done and provide a detailed explanation of the rationale for each repeated test in your billing documentation in a very clear way.
| Aspects | 59 | 25 | 91 |
| Description | Used to distinguish a procedure or service from other services performed on the same day. | Indicates a significant, separately identifiable evaluation and management (E/M) service. | Healthcare providers use Modifier 91 when they repeat a laboratory test on the same day to obtain multiple test results. |
| Purpose | To prevent improper bundling of services that are distinct and separate. | It serves to distinguish the additional assessment and management that are part of the same visit. | Distinguish additional tests conducted to obtain multiple results for the same laboratory test. |
| Examples | A patient receives two injections in different muscles on the same visit, | A patient undergoes a minor surgical procedure, such as wart removal, and separately experiences an evaluation for an unrelated condition in the same visit, | A doctor performs several x-rays or scans in a single day for the tracking of the progression of a disease or to control the precision of the results |
| Mistakes to Avoid | Overuse of Modifier 59Unbundling without any reasonLack of Documentation | Failure to Link E/M Service to Other ProceduresIncorrect Code Selection for E/M ServiceInsufficient Documentation of Separate E/M Service | Fails to Document Specific Clinical NecessityInappropriate Use in Relation to Other Modifiers or Procedure CodesLack of Specificity in Identifying Repeated Tests |
Conclusion
Knowing the medical billing modifiers in detail is very important for healthcare providers to facilitate proper reimbursement and compliance with coding guidelines as well. In this blog, we’ve explored three commonly used modifiers: 59, 25, and 91. Awareness of the specific scenarios in which modifiers are applicable to healthcare providers can enable them to achieve perfect billing accuracy. Moreover, it helps prevent claim denials and obey guidelines for coding. Thorough documentation, coupled with the right use of modifiers, and excellent communication with the payers will serve as the foundation for successful medical billing.