Over the past two decades, healthcare has undergone a major digital transformation, shifting from paper charts to advanced electronic systems. This evolution has significantly improved patient care coordination, accessibility, and accuracy.
However, as healthcare practices continue to adopt new technologies, one question remains:
What’s the difference between an Electronic Health Record (EHR) and an Electronic Medical Record (EMR)?
At first glance, these terms may seem interchangeable, but they represent two distinct systems with unique features and impacts on patient care. Understanding the differences between EHR and EMR goes beyond technical terminology — it’s a crucial step in enhancing workflow efficiency, ensuring data accuracy, maintaining compliance, and improving long-term patient outcomes.
What is an Electronic Medical Record (EMR)?
An Electronic Medical Record (EMR) is a digital version of a patient’s paper chart used within a single healthcare practice or organization. It contains clinical notes, diagnoses, treatment plans, and medical histories — all managed electronically to simplify daily operations. The primary purpose of an EMR is to enhance record accuracy and efficiency for healthcare providers working in the same clinic or hospital.
Key functionalities of an EMR:
Charting and Documentation: Providers can record patient visits, diagnoses, prescriptions, and progress notes in a structured digital format.
Patient Tracking: EMRs allow clinicians to monitor lab results, treatment history, and preventive screenings over time.
Clinical Decision Support: Many EMRs include reminders or alerts for routine checkups, vaccinations, or patient drug interactions.
Limitations:
Although EMRs streamline internal processes, they are limited to a single practice or organization. They do not readily share information with other healthcare systems, so their records do not follow if a patient visits another provider. This lack of interoperability often makes it difficult for different healthcare professionals or facilities to coordinate care effectively.
Example:
Consider a family physician using an EMR to manage patient records. The system lets them quickly access each patient’s medical history, update prescriptions, and track lab results. However, the new test results and specialist notes won’t automatically appear in the family doctor’s EMR if the same patient visits a cardiologist in a different network.
What Is an Electronic Health Record (EHR)?
An Electronic Health Record (EHR) is a comprehensive digital record of a patient’s health information that can be shared securely across different healthcare organizations. Unlike EMRs, which are confined to one practice, EHRs are designed for interoperability — enabling providers, specialists, and hospitals to access and update patient data in real time. EHRs often include lab results, imaging, medications, allergies, demographics, and treatment histories, offering a complete view of the patient’s health journey.
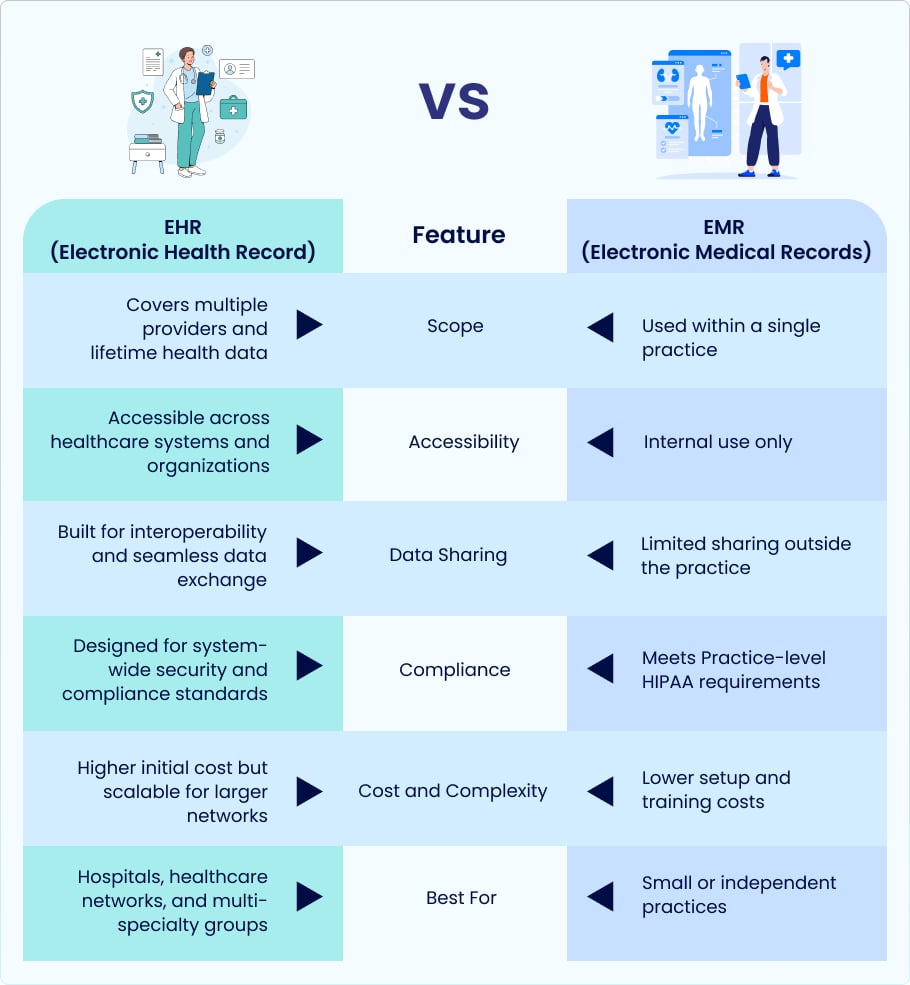
EHR vs. EMR: A Comparative Overview
When choosing the right system for your healthcare practice, it’s crucial to understand the differences between EHRs and EMRs. Both store digital health information but vary significantly in scope, functionality, and accessibility. The table below highlights their key distinctions.
EMRs focus on improving internal record-keeping within one practice, while EHRs connect the entire healthcare ecosystem, enabling coordinated, data-driven, and patient-centered care.
EHR and EMR technologies have transformed how medical professionals deliver, document, and coordinate patient care. While EMRs improve accuracy within a single practice, EHRs extend those benefits across the broader healthcare network by enhancing patient engagement, collaboration, and data-driven insights.
Improved Care Coordination
EHR systems enable multiple clinicians to access and update a patient’s information in real time, eliminating data silos. With this integrated approach, every specialist involved in a patient’s care — from primary care physicians to cardiologists and endocrinologists — can view the same up-to-date information.
Example:
EHRs provide quick access to lab results, medication histories, and treatment updates for all clinicians managing chronic conditions such as diabetes or heart disease. This reduces duplicate testing, strengthens communication, and helps the care team make more informed and consistent decisions.
Data-Driven Clinical Decision Support
Modern EHRs include AI-driven analytics and Clinical Decision Support Systems (CDSS) that help physicians make faster, more accurate decisions. These tools analyze patient data in real time and alert providers to potential drug interactions, missed screenings, or abnormal test results.
EHRs with predictive analytics can also identify at-risk patients before complications develop, enabling proactive rather than reactive care. While EMRs remain valuable for documentation, they generally lack the advanced analytical and cross-system capabilities that EHRs provide.
Patient Engagement and Accessibility
EHRs have transformed the patient experience by offering instant access to health data through mobile apps and secure online portals. Patients can communicate with their clinicians, schedule appointments, and view results — all from a single platform.
This level of transparency encourages patients to take an active role in their care, leading to greater treatment satisfaction and adherence. In contrast, EMRs limit access to in-office visits, offering fewer opportunities for ongoing engagement or self-management.
Regulatory and Reporting Advantages
EHR systems are vital in meeting federal reporting and compliance requirements such as Meaningful Use, MIPS, and MACRA (Medicare Access and CHIP Reauthorization Act). They excel in patient engagement, data exchange, and outcome improvement — all recognized and rewarded under these programs.
While EMRs comply with HIPAA standards at the practice level, they lack the automated reporting and interoperability needed for system-wide compliance and participation in government incentive programs.
These programs, established by the Centers for Medicare & Medicaid Services (CMS), incentivize practices that demonstrate meaningful use of certified EHR technology.
Choosing Between EHR and EMR: Which is Right for Your Practice?
Choosing the right digital record system directly impacts productivity, patient experience, and long-term growth. The choice between an EHR and an EMR is more than a technical decision — it depends on your practice’s structure, interoperability goals, and future scalability.
Key Factors to Consider
Practice Size and Specialization:
An EMR can be a practical choice for smaller or single-specialty practices because it’s easier to implement and manage within one location. However, larger or multispecialty organizations need the networking and coordination capabilities only EHRs can provide.
Budget and Infrastructure:
EMRs generally have lower upfront costs and require less IT support. EHRs, on the other hand, may involve higher initial investment, but their automation, analytics, and interoperability deliver greater long-term benefits.
Interoperability Needs:
An EHR is a smarter choice if your clinic often exchanges data with outside labs, hospitals, or specialists. EMRs don’t have the built-in data interchange capabilities needed for smooth coordination.
Scalability for Future Growth:
Consider your five-year growth and scalability goals. EMRs are more suited for small-group or single-site use but provide flexible cloud options that can expand with your company.
Here’s a quick recommendation chart:
| Practice Type | Recommended System |
| Solo Practice | EMR |
| Group Practice/Hospital | EHR |
| TeleHealth /Multi-site Network | Cloud-based EHR |
What to Look for in an EHR/EMR System
- Ease of use and intuitive interface
- Interoperability with labs, payers, and pharmacies
- Built-in compliance with HIPAA and 21st Century Cures Act
- Scalable cloud infrastructure
- AI and analytics support
- Vendor support, training, and customization options
Integration and Interoperability: The Real Game-Changer
In today’s connected healthcare environment, integration and interoperability are no longer optional — they’re essential. The real strength of an EHR lies in its interoperability — its ability to connect seamlessly with other systems so that patient data flows securely and efficiently across every stage of the care process.
Interoperability Standards: FHIR and HL7
Latest EHR systems rely on Interoperability standards such as HL7 (Health Level Seven) and FHIR (Fast Healthcare Interoperability Resources) to enable smooth data exchange between platforms.
- HL7 provides the foundational framework that allows healthcare applications to share clinical and administrative data.
- FHIR, a newer standard, simplifies this exchange by using web-based APIs, making it easier for systems — even mobile apps — to access and share real-time patient data.
These standards ensure EHRs can connect labs, pharmacies, imaging centers, and payers without compatibility issues.
How EHRs connect the Healthcare Ecosystem
EHR integration bridges the gap between multiple touchpoints in a patient’s care journey. For example:
- Labs can automatically send test results directly to the provider’s EHR.
- Pharmacies can receive electronic prescriptions and share medication adherence data.
- Payers can verify eligibility, process claims faster, and support value-based care reporting.
This connected workflow reduces errors, improves turnaround times, and enhances overall care coordination — something traditional EMRs cannot achieve simultaneously.
Real-World Example: EHR integration in Medication Reconciliation
Consider a patient who visits multiple doctors, each prescribing different medications. Poor communication can result in inconsistent or duplicate prescriptions. An interoperable EHR automatically compiles pharmaceutical data from physicians and pharmacies into a unified record. When the primary care physician reviews the patient’s information, the system alerts them to potential drug interactions or duplications, ensuring safer and more accurate medication management.
EHR vs. EMR and Revenue Cycle Management (RCM)
Beyond clinical documentation, EHR and EMR systems play a vital role in revenue cycle management (RCM) by ensuring accurate billing, proper coding, and timely reimbursement. However, each system’s level of automation and support can vary significantly.
How Each System Supports Billing and Claims
EHRs and EMRs help providers document patient visits, record charges, and export billing data for claim submission. These systems minimize administrative errors and payment delays by streamlining processes such as charge capture, claim tracking, and accurate coding. However, the extent to which you integrate revenue cycle management (RCM) workflows depends on whether you use an EHR or an EMR.
EHR’s Advantages: Integrated RCM Dashboards and Eligibility Checks
Modern EHR systems go beyond documentation and often include integrated RCM solutions that automate billing. Through connected dashboards, staff can verify patient eligibility, confirm coverage, and track claim status in real time. Many EHRs also offer analytics that identify denial trends, payment delays, and coding errors, allowing practices to manage revenue performance proactively.
This end-to-end visibility enables providers to connect clinical data with financial outcomes, supporting value-based care and ensuring accurate reimbursement.
EMR’s Limitation: Dependence on Third-Party Billing Modules
EMRs, on the other hand, typically focus on clinical documentation within a single practice and may not fully integrate with billing operations. Practices often rely on third-party billing services or external software to handle insurance claims and reporting, which can create data silos and inefficiencies. Although this setup may work for smaller practices, it limits scalability and makes reporting more challenging when data needs to be shared across multiple systems.
Security and Compliance in Digital Health Records
Security and compliance have become top priorities for all healthcare providers as patient data moves online. Federal privacy laws such as HIPAA require strict protection of patient information and secure management of EHR and EMR systems to prevent unauthorized access. However, each system handles these responsibilities differently.
HIPAA Compliance, Encryption, and Access Controls
EHRs and EMRs must comply with the Health Insurance Portability and Accountability Act (HIPAA) to protect sensitive patient data. This includes features like:
- Data Encryption: Ensuring that all patient records, whether stored or transmitted, remain secure and unreadable to unauthorized users.
- Access Controls: Limiting data visibility to authorized staff based on their role or responsibility.
- Audit Trails: Maintaining detailed logs of who accessed, modified, or shared patient information.
These measures help prevent data breaches, identity theft, and unauthorized disclosures — risks that can carry severe financial and reputational penalties.
Patient Consent and Data Portability under the 21st Century Cures Act
The 21st Century Cures Act strengthens patient rights by promoting data privacy and transparency. Under this law, healthcare providers must give patients prompt electronic access to their medical records upon request. The act also strongly emphasizes patient consent, ensuring individuals have full control over who can access or share their data.
With their built-in interoperability, EHR systems naturally align with these standards by enabling secure data sharing among different systems and providers without compromising privacy. In contrast, EMRs often lack integrated features that support seamless patient access and external data exchange.
This aligns with the U.S. Department of Health and Human Services (HHS) information-blocking rules, which mandate timely patient access to health data.
EHR’s Advantage: Centralized Compliance Monitoring
One key advantage of modern EHRs is centralized compliance management. These systems include dashboards that track audit activity, detect security risks, and ensure compliance with evolving legal requirements.
This proactive approach allows healthcare organizations to maintain patient trust, stay audit-ready, and avoid costly compliance penalties. In contrast, EMRs — limited to a single practice — often require manual monitoring or external tools to achieve the same level of oversight.
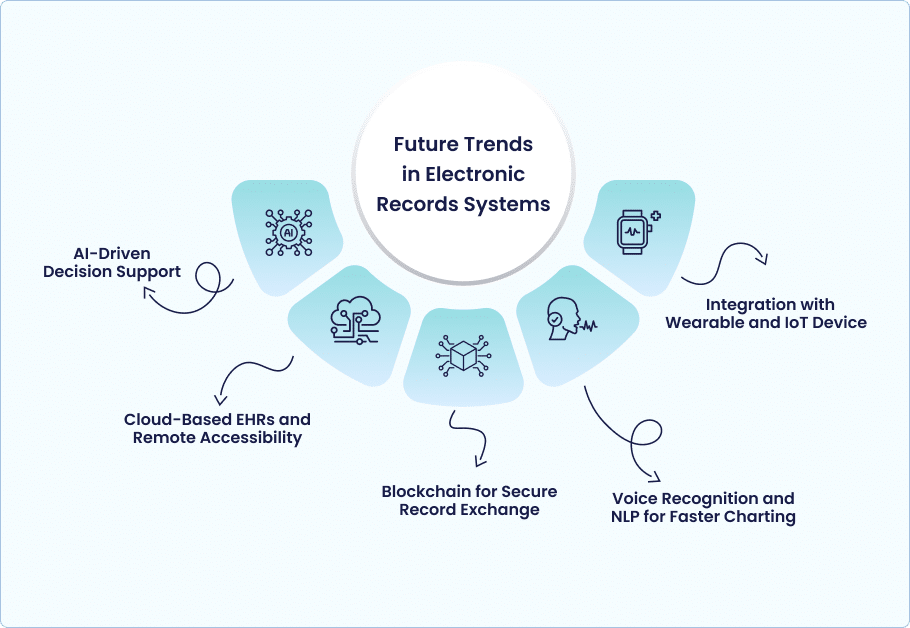
Future Trends in Electronic Records Systems
Electronic record systems evolve rapidly as technology reshapes how healthcare data is shared, managed, and analyzed. Beyond documentation, the next generation of EHR and EMR systems will focus on intelligence, connectivity, and real-time insights that improve provider efficiency and patient outcomes.
AI-Driven Decision Support
- AI is transforming EHRs into intelligent clinical assistants through predictive analytics and automation
- Future EHR systems will include AI-powered decision support tools.
- Predictive analytics will help identify patient risks early.
- AI recommendations will assist providers in choosing optimal treatment options.
- Error detection capabilities will help catch potential clinical or documentation mistakes before they occur.
- Automation of routine tasks like documentation and coding will reduce administrative burden.
- Overall outcome: enhanced clinical accuracy, efficiency, and workflow optimization.
Cloud-Based EHRs and Remote Accessibility
- Cloud technology is making EHRs more accessible, flexible, and scalable.
- Providers can securely access patient data from any device or location.
- This accessibility is crucial for telehealth, multi-site practices, and remote care teams.
- Cloud-based systems simplify software updates, data backups, and disaster recovery.
- These capabilities improve efficiency, reliability, and continuity of care.
Blockchain for Secure Record Exchange
- Blockchain technology offers substantial potential for enhancing healthcare data security.
- It creates tamper-proof, decentralized records that protect patient information.
- Data shared between systems remains authentic, traceable, and verifiable.
- Blockchain can reduce or eliminate security risks linked to traditional data exchange methods.
- This innovation promotes trust, transparency, and integrity in health information management.
Voice Recognition and NLP for Faster Charting
- Voice recognition and Natural Language Processing (NLP) are transforming clinical documentation.
- Providers can dictate notes directly into the EHR instead of typing manually.
- The system enables real-time transcription and structured data capture.
- This technology reduces documentation time and administrative workload.
- It frees providers to focus more on patient care and meaningful patient interactions.
Integration with Wearable and IoT Devices
- Future EHR systems will integrate with wearables and IoT-enabled health devices.
- Examples include smartwatches, fitness trackers, and home monitoring sensors.
- These devices will continuously collect health data such as heart rate, glucose levels, and blood pressure.
- Data will feed directly into the patient’s electronic record in real time.
- This integration will provide clinicians with continuous insights into patient health.
- It will enable preventive, personalized, and data-driven care.
Conclusion
Electronic Medical Records (EMRs) are digital versions of traditional paper charts, primarily used for documentation within a single practice. EHRs, on the other hand, form part of an interconnected, interoperable health ecosystem that supports data-driven and coordinated care across multiple providers and care settings.
As healthcare technology continues to evolve, choosing the right EHR or EMR system is vital to staying compliant, efficient, and patient-focused. Evaluate your organization’s needs carefully — and consider adopting a future-ready EHR solution that enhances care coordination and drives better outcomes.