In the modern world, the need for mental and behavioral health services has increased tremendously. But even with an augmented need for care, a frustrating hurdle can stand between patients and the treatment they deserve: insurance claim denial. These denials can not only affect the patient’s care journey but also have an impact on your organization’s revenues. However, there’s good news!
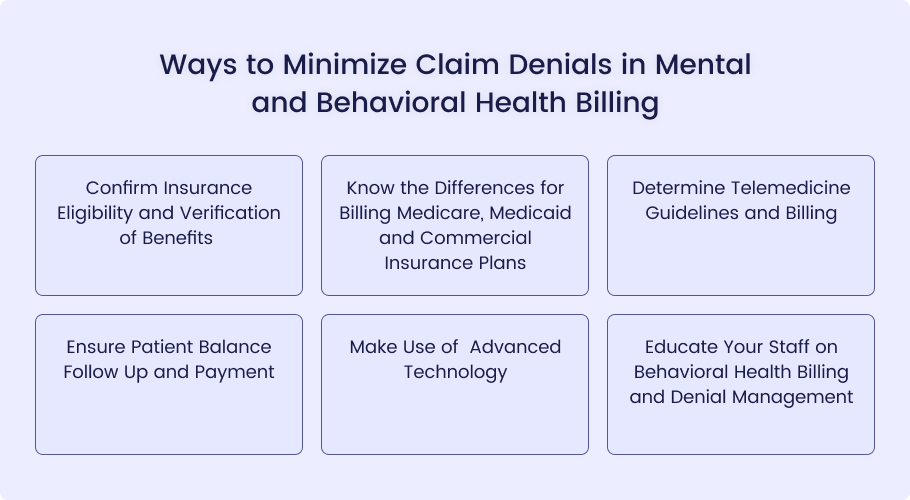
Below are some strategies that your mental and behavioral health organization can put in place to minimize the number of claim denials and, hence, make the process easier for both the healthcare providers and the patients.
Mental and behavioral health billing is the process of filing insurance claims for services that have been given by psychologists, therapists, psychiatrists, and other behavioral health care providers. However, it has some peculiarities when compared to conventional medical billing. These include things like the coding of psychotherapy sessions depending on the time spent in the session, checking whether the patient is covered for a certain type of session due to certain restrictions, and changes in insurance rules that may be quite different from those of general medical practice.
Following are some of the effective strategies to minimize claim denials, and hence, improves the overall financial health of your mental and behavioral health facility.
Also Read: Common Mistakes for Insurance Denials and How to Avoid Them
Confirm Insurance Eligibility and Verification of Benefits
Behavioral health services are often provided by out-of-network professionals as compared to other healthcare services. It is therefore important to double check the details of the patient’s insurance prior to initiating treatment to avoid confusion and ensure that the billing process is hassle-free.
This involves two key steps: First, verifying the authenticity and current validity of the insurance policy stated, and second, the details of the benefits that the plan offers. Some of the things to consider include annual visit caps, pre-authorization needs, and out-of-pocket expenses.
This way, you can devise a proper payment structure so that there are no misunderstandings and financial pressure on both the patient and yourself.
Know the Differences for Billing Medicare, Medicaid and Commercial Insurance Plans
Behavioral health billing has several layers of rules and guidelines because of the variances between private and government insurance providers. These payers have different code sets, legal standards, and ways of submitting claims for bills.
This is further compounded by the fact that some codes are used differently depending on the payer type, and even within the payer types, some codes may need different modifiers. This can lead to claim denials, which is not only frustrating but also time-consuming and costly.
In order not to face denials, behavioral health practices should ensure that they gain knowledge of the rules of each payer and provider type for each patient.
Determine Telemedicine Guidelines and Billing
The use of telemedicine is rapidly increasing, especially in the behavioral health sector, with the market size expected to reach $324 billion by 2030. This growth is attributable to the rising need for behavioral health services and the ease of access that telemedicine provides.
However, the rules concerning the insurance of telemedicine services are changing frequently. It becomes important for the providers to stay updated with these changes, especially to avoid claim denial and get proper reimbursement.
Therefore, mental health practices should ensure they follow the changing policies in order to have a good cash flow and still be able to deliver care through telemedicine.
Ensure Patient Balance Follow Up and Payment
Mental health services are often provided by out-of-network providers, which means that patients are often left to pay the high costs of treatment. To handle this delicate situation, one has to be very careful and consider the patient’s needs as the primary concern.
It is recommended that practices tailor their communication with patients to their financial circumstances. Accepting payment methods such as cash, check, credit, and online will be helpful in this case.
Moreover, payment plans set during registration and based on the benefit levels can be useful for patients to pay for out-of-pocket costs.
Make Use of Advanced Technology
Complicated billing should not be a problem for you! Integration of technology is important in behavioral health practices as it can greatly improve their operations. Choose an EHR that can easily integrate with your billing software for efficient service delivery. This facilitates fast coding from the patient notes within the EHR, with a low possibility of making mistakes.
For instance, adopt the electronic billing that insurance firms provide in a bid to hasten the claims to be lodged and also to avoid the loss of paper-type claims. It is recommended to negotiate with a clearinghouse service to perform certain functions automatically.
Clearinghouses can accept and process claims, check eligibility, and even manage denials, which saves much-needed time for other processes.
Educate Your Staff on Behavioral Health Billing and Denial Management
Ensure that your staff understands the challenges of behavioral health billing and denial management to prevent future occurrences. This training should preferably be geared towards the needs of behavioral health payers and may include information on the use of ICD-10 and CPT codes in the behavioral health setting.
The staff should be familiar with the criteria for medical necessity related to behavioral health interventions and the documentation that would support the treatment plans and the patient outcomes.
This way, your team will be up-to-date with the changes in the legal framework and industry standards and reduce the chances of denial due to improper coding or a lack of documentation.
To improve your revenue cycle management and enhance your reimbursement, it is advisable to consider working with a professional medical billing company such as Medheave. The process of handling behavioral health billing is quite complex due to the constant changes in laws and rules, and it can strain your internal team.
Medheave can provide end-to-end billing services, including verifying eligibility, submitting claims, handling denials, and collecting patient balances. This allows your practice to focus on what matters most: consistently producing superior mental and behavioral health outcomes for your patients.
Contact Medheave-Medical Billing Services for expert assistance at (888) 487-1178