
Medicaid is the nation’s public health insurance program. It opens up opportunities for healthcare providers to serve a diverse range of populations. Any error during the Medicare enrollment or credentialing process can put a physician in hot water. His contract with the State Medicaid Agency can be terminated, leaving him unable to get paid.
This guide helps healthcare providers understand everything related to Medicaid credentialing. From basics to strategies, uncover the process, benefits, and FAQs in one place.
Understanding Medicaid welfare Program in USA
- Medicaid is a jointly funded federal-state health program in the USA. Low-income, needy people are eligible to enjoy medical assistance under this program.
- More than 90 million individuals, including children, disabled persons, and the elderly, are provided coverage. People who receive federally assisted income maintenance payments are also covered.
- The Center for Medicare and Medicaid Services (CMS) is responsible for managing the enrollment process.
- In the state fiscal year 2021, Medicaid accounted for 27% of total state expenditures. 45% of expenditures come from federal funds, and 15% of expenditures come from state funds.
What is Medicaid Credentialing?
Medicaid credentialing is the process of validating the eligibility of healthcare providers. They get approval to bill the Medicaid program for services rendered to the needy and low-income individuals.
Credentialing makes sure that the provider meets the legal standards of the Medicare agency. It checks the qualifications for participating in Medicaid programs.
The process includes verification of the provider’s educational background. Work experiences, licensure, certifications, professional references, etc. are also validated.
Medicaid Credentialing Requirements
Medicaid credentialing requirements vary from state to state. But some common elements that are followed by everyone are listed below.
Healthcare providers must have:
- National Provider Identifier (NPI) number
- Tax ID Number (TIN)
- Social Security Number (SSN)
- Professional license
- Specified educational background and certifications
- submit a complete enrollment application to the state Medicaid agency.
- comply with all the rules and guidelines of the Medicare agency.
- pass a criminal background check to ensure security and patient safety.
- practice location must be within the state where he is enrolled in Medicaid.
Credentialing Process for Physicians
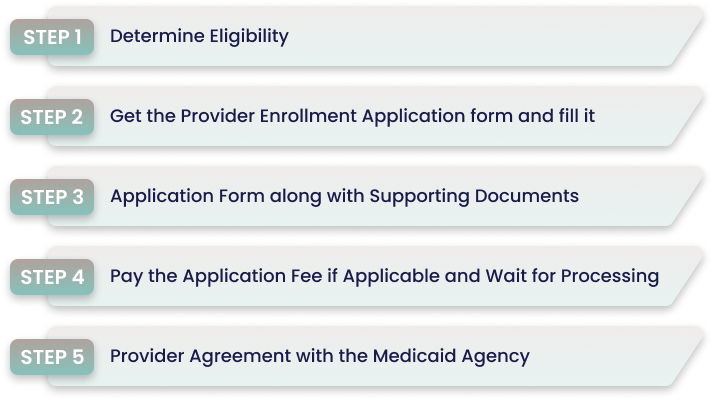
Step 1 Determine Eligibility
Ensure that the physician fulfills the eligibility criteria set by the state Medicaid. This includes obtaining a National Provider Identifier (NPI) and a Tax Identification Number (TIN). Holding a valid license and having an appropriate educational background is also validated .
Step 2 Get the Provider Enrollment Application form and fill it
The application form for provider enrollment varies by state. Contact your state’s Medicaid program agency and fill out the form appropriately. Provide details such as education, practical experience, references, etc.
Step 3 Submit Application Form along with Supporting Documents
Gather all the necessary documents. This includes copies of professional certifications, diplomas, license and any other document specified by the state Medicaid agency. Submit all the documents along with the application form to the designated address.
Step 4 Pay the Application Fee if Applicable and Wait for Processing
Pay the dedicated application fee if your state charges it. Allow the Medicaid agency to verify your application and documents. The processing time varies, ranging from a few weeks to several months.
Step 5 Provider Agreement with the Medicaid Agency
Once approved, you need to sign an agreement with the state Medicaid agency. All the rules regarding participation in the Medicaid program are properly mentioned. After receiving an approval notification, you can start providing services to Medicaid beneficiaries.
Also Read: Reasons to Outsource Medical Credentialing
Benefits of Medicaid Credentialing for Healthcare Provider
Authorized for Medicaid Services
Through medical credentialing, providers are authorized to deliver services covered by the Medicaid Program. The authorization process is crucial for provider participation in the program. This helps to receive financial coverage for services rendered to the beneficiaries.
Meet Specific Quality Standards
The credentialing process involves the confirmation of the provider’s educational background. His certifications and training are also verified. By doing this, the provider meets the quality standards set by the Medicare agency.
Broader Patient Reach
Many individuals, such as the elderly, needy, low-income, and children, rely only on Medicaid for healthcare services. Inclusion in these programs enhances the patient’s reach.
Enhances the Provider’s Credibility and Reputation
Participation in government-funded healthcare programs enhances the reputation and credibility of the provider. Affiliation with Medicare ensures that the provider is committed to providing standard patient care and covers a diverse range of patients.
Strategies to Optimize the Medicaid Credentialing Process
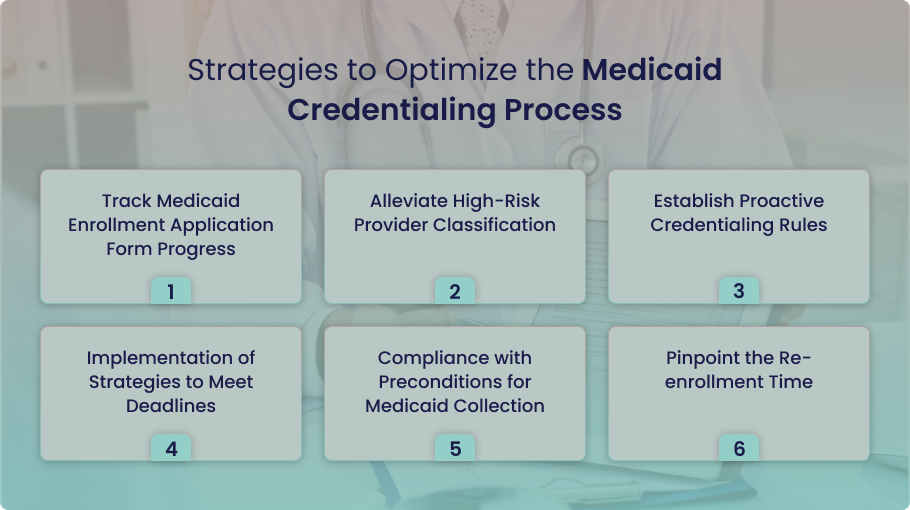
Track Medicaid Enrollment Application Form Progress
Track the status of your enrollment application form. This allows you to stay informed about any issue, and you can take prompt action.
Alleviate High-Risk Provider Classification
Mitigate the reasons to be classified as a high-risk provider by the Medicaid agency. Implement strategies that can safeguard your professional reputation.
Establish Proactive Credentialing Rules
Proactive credentialing rules save you from threats of termination from the Medicaid program.
Implementation of Strategies to Meet Deadlines
Implement a strategic plan to manage the credentialing process before the last date. This helps you to be compliant with Medicare’s requirements and deadlines.
Compliance with Preconditions for Medicaid Collection
For financial stability, understand the preconditions set by the Medicare agency. Payment collection becomes feasible once compliance is assured.
Pinpoint the Re-enrollment Time
Pinpoint the re-enrollment application time to avoid fines and penalties. This also helps to avoid any delay in the Medicare enrollment process.
FAQs
What should I do if my Medicaid Credentialing Application is Denied by Medicaid?
If your application is denied, you will receive a notification from Medicaid. The notification will highlight the reason behind the denial. You can appeal or reapply once you address the issue.
Is the Medicaid Credentialing Process Different in Each State?
Yes, every state administers its own Medicaid credentialing process. A healthcare provider must be aware of the variations and follow the requirements of their state.
What is Revalidation in Medicaid Credentialing?
Revalidation is the process of validating and updating the provider’s information at regular intervals. This helps the provider be compliant with Medicaid’s basic requirements.
Can I Check the Status of my Medicaid Credentialing Application Form?
Yes, you can check the status of your Medicare credentialing application. Many states provide online portals or hotlines. Contact your state’s Medicaid agency number and confirm it.
What Steps are Necessary if I Want to Practice Across Multiple States?
Firstly, make yourself familiar with the customized Medicaid program’s requirements in each state. Then apply for enrollment in each state separately.
Conclusion
Medicaid credentialing validates the eligibility of healthcare providers to obtain approval to bill the Medicaid program for services rendered to the needy and low-income individuals. Although the process is complex and time-consuming, it allows the healthcare provider to be authorized for Medicaid services. It helps them meet specific quality standards and broadens their patient’s reach. The provider’s credibility and reputation are also enhanced.
At Medheave, we enable healthcare providers to deliver care to Medicaid beneficiaries while getting reimbursed for all the services. Partner with Medheave and enjoy the timely credentialing process. Contact us today for further details.




