As a laboratory or diagnostics business owner, you already know the importance of running accurate and efficient lab tests. But what happens when you send those test results to insurance companies for reimbursement?
That’s where the lab billing process comes in. It’s a bit like the back office of your business—the less you focus on it, the more you might face issues with cash flow and getting paid on time.
Laboratory billing, at its core, is about ensuring your services are properly documented, coded, submitted to insurers, and reimbursed correctly.
It’s similar to the medical billing practices in hospitals or private practices, but there are unique challenges that lab owners face, especially when it comes to keeping up with ever-changing regulations, coding standards, and payer requirements.
In this blog, we will discuss some major challenges and complexities that a lab may encounter. Additionally, we will give you the best solution to tackle these challenges in the form of our expert laboratory billing guidelines to make things smooth and efficient for lab RCM management.
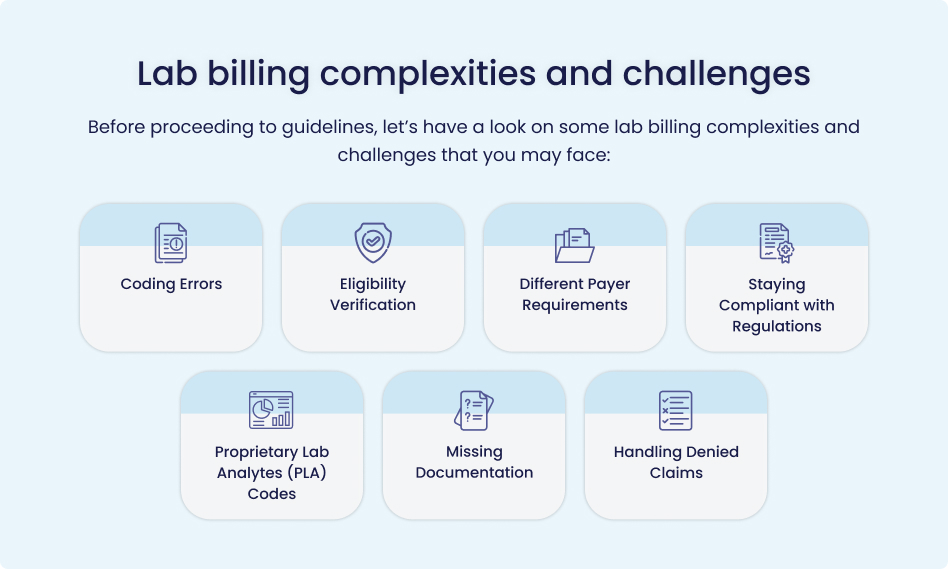
Coding Errors
Coding errors in pathology and laboratory services are among the most common issues faced by lab owners. Even minor mistakes, such as selecting the wrong test code or omitting a necessary diagnosis code, can lead to claim rejections.
A simple misstep, such as incorrectly coding a blood test, could take weeks before it’s flagged by the insurance company, causing a delay in payments and extra work to correct the mistake.
Eligibility Verification
Failure to verify a patient’s insurance eligibility before conducting tests can result in unreimbursed procedures, adding to financial strain.
Without this verification, you could end up performing tests for patients whose insurance is no longer active, leaving you to chase them for payment.
Different Payer Requirements
Each insurance company has its own unique requirements like different forms, rules, and documentation requirements.
| What is CLIA and How to Use It?
A CLIA (Clinical Laboratory Improvement Amendment) number is a unique identifier required for certain laboratory tests. It is important for proper claim submission and reimbursement. THE format of a CLIA number is 19DXXXXXXX. The first three characters are the two-digit state code followed by the letter D. The remaining seven digits are the unique CLIA system number assigned to the provider. Do not add the letters CLIA to the 10-character CLIA number. FOR MORE INFORMATION CLICK HERE: |
For lab managers different requirements can feel like learning a new language.
For example, Medicare might ask for specific documentation for a test that a private insurer doesn’t. If you miss these details, your claim could be denied.
Staying Compliant with Regulations
Another significant challenge is staying compliant with evolving healthcare regulations. Compliance is non-negotiable, as violations can result in heavy fines. For example, not following HIPAA guidelines for patient data can lead to both legal and financial consequences.
If you are not adhering to HIPAA guidelines when handling patient data can lead to serious legal and financial consequences.
Proprietary Lab Analytes (PLA) Codes
The use of Proprietary Lab Analytes (PLA) codes for laboratory-developed tests introduces an extra layer of complexity to the billing process. Forgetting to use the correct PLA code can prevent reimbursement, highlighting the importance of accuracy in all aspects of billing.
For example, if you perform a specialized genetic test using a proprietary method but forget to use the corresponding PLA code, your claim could be denied, impacting revenue.
Missing Documentation
Missing documentation is another common cause for delayed or denied claims. Every claim needs to be supported by complete and accurate documentation. If something is left out, such as a physician’s order for a test, your claim will be rejected, forcing you to gather and resubmit the missing information.
Handling Denied Claims
All above discussed issues then cause claim denials. Hence, the laboratory managers might find themselves in trouble while handling denied claims if they are increasing.
But. if your claim is denied, it doesn’t mean the process is over.
You’ll need to figure out why it was rejected, correct any issues, and submit an appeal.
This takes time, and it can be stressful.
If a test gets denied because the diagnosis code doesn’t match the procedure, you’ll have to correct the code, write an appeal letter, and resubmit the claim, which adds to your workload.
Ultimately, these complexities and issues in Lab billing and RCM process destroy the whole cash flow of a lab and leaves lab owners in stress.
To address these challenges and issues, lab owners must have a strategic roadmap.
They should streamline the whole billing process for maximum collection of lab revenue and ensure patient satisfaction as well.
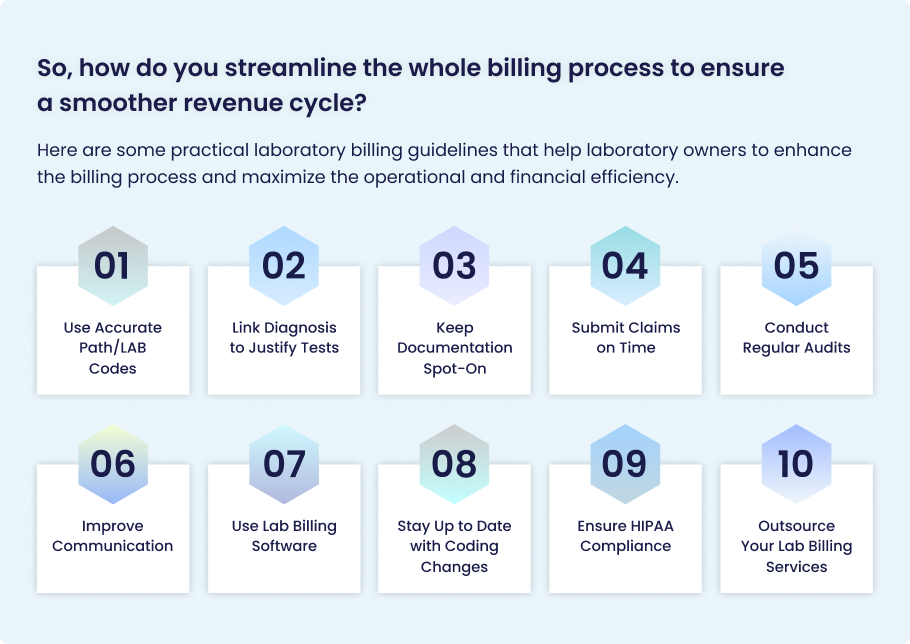
Use Accurate Path/LAB Codes
This one is non-negotiable. Using the right Lab CPT codes for each test is essential. Don’t guess—make sure the code you use precisely matches the service provided.
If you’re testing for a rare genetic condition, make sure the exact test code is used, not just a general code for genetic testing.
Link Diagnosis to Justify Tests
You need to back up each test with the correct ICD-10 diagnosis code. Insurance companies usually confirm that the tests were necessary and then accept claims for reimbursements.
For instance, if you are conducting a cholesterol test, link it to an ICD-10 code indicating the patient’s risk factors for cardiovascular disease to justify the medical necessity of the test.
Keep Documentation Spot-On
Accurate records are your best friend. Keep detailed logs of every test, patient information, and physician orders.
Make sure the order from the doctor for a CT scan is included with the claim submission. Missing that order is a common reason for denials.
Submit Claims on Time
Don’t let deadlines pass. Many insurers require claims to be submitted within 30 days or less, so the faster you submit, the better.
If an insurance company requires claims within 14 days of service, ensure that your billing team gets claims out the door ASAP.
Conduct Regular Audits
Regular internal audits are a good practice. They help you catch coding mistakes, billing errors, or compliance issues before they turn into big problems.
Review your most common procedures every quarter to ensure the codes you’re using are still up to date.
Improve Communication
Encourage communication between your lab techs, physicians, and billing department. Clear and accurate information is critical for correct claim submissions.
If a physician orders a test with specific instructions, ensure the billing department knows about it to avoid mistakes on the claim.
Use Lab Billing Software
Utilizing an efficient lab billing software that integrates with your electronic health records (EHR) can automate much of the billing process and reduce manual errors.
Also, automate the eligibility verification process to reduce the errors in basic patient and payer information during the eligibility verification process.
Use software that auto-populates ICD-10 and CPT codes for lab billing based on the test type, which will save time and minimize human error.
Stay Up to Date with Coding Changes
The medical coding world doesn’t stand still. Ensure your team is aware of any changes to CPT, ICD-10, and payer policies.
Attend coding webinars or subscribe to updates from coding authorities so you’re always in the loop.
Ensure HIPAA Compliance
Protect patient information by strictly following HIPAA guidelines. Not just for the sake of legality, but to maintain trust with your patients.
Make sure your billing system is secure and only accessible by authorized personnel.
Outsource Your Lab Billing Services
If you’re handling everything yourself and feeling stressed, hiring an outsourced billing company might be worth the investment.
Consider outsourcing the lab billing and coding tasks to expert Lab billing and RCM services. This can save time and ensure accuracy.
Final Thoughts
In a nutshell, laboratory billing may seem like a complicated task, but with the right strategies and following above given laboratory billing guidelines, you can streamline the process, avoid mistakes, and ensure timely reimbursements. Focus on accuracy, stay up-to-date with the latest guidelines, and always ensure clear communication between your team. This approach will help you reduce the financial strain caused by billing errors and keep your lab’s cash flow healthy.
| Partner with Medheave for Excellent Lab Billing Services
Medheave is an expert lab billing service provider in the USA. Let Medheave handle your complex lab billing tasks to enable you to focus on accuracy in lab tests. As experts in lab billing, we ensure accurate coding, timely claim submissions, and compliance with all regulations, so you get paid faster and without the hassle. Contact Medheave today and experience a smoother, more efficient billing process for your lab. |