Have you ever tried to find out what CO 197 means when you are informed that your medical claim has been denied? This unassuming string of characters and digits can have physicians or other healthcare practitioners baffled and pondering about the causes of mishaps. But fear not! This ultimate guide will serve as your all-in-one resource for the CO 197 denial code and possible ways of avoiding it.
Denial Code CO 197 indicates that a required pre-authorization, notification, or certification was not completed before the claim submission. This code signals that the necessary approval or notification from the insurance company or other relevant entities was missing prior to providing the medical service or procedure. As a result, the claim is denied due to this lapse in authorization.
Pre-authorization: This is a legal process whereby a healthcare provider asks permission from the insurer to do a particular service on behalf of a policyholder or patient. The healthcare physician prepares a written justification for the service that is to be provided, together with expected charges and the medical necessity supporting the same.
Notification: In some cases, the insurance company may simply need to be informed regarding certain procedures, even if a formal pre-certification is not necessary. This might include notifying the insurance company before a service is to be rendered, but it is not as elaborate as a precertification request.
Certification: In some cases, some processes may need a doctor’s approval to verify that the procedure is needed medically. This certification is then submitted, accompanied by the claim that the services would support coverage.
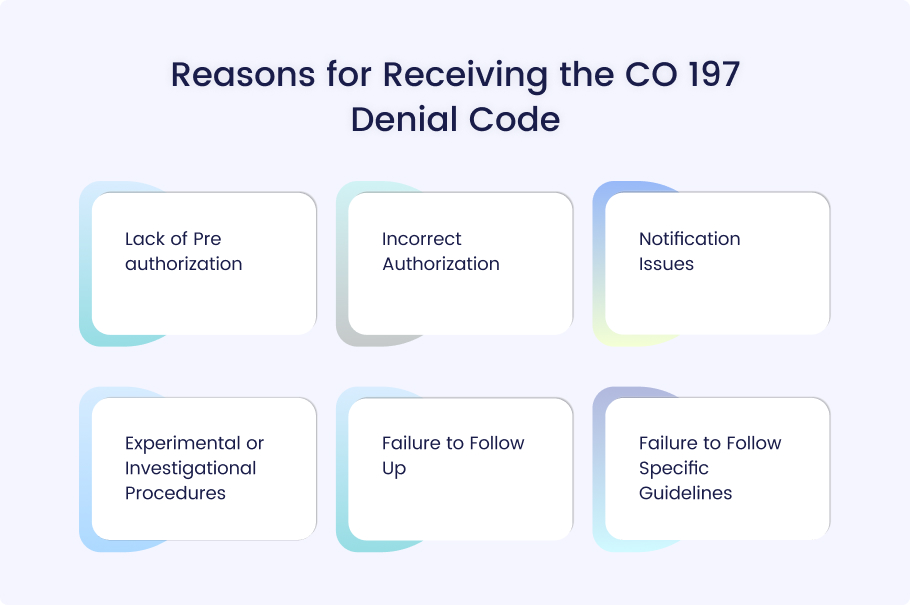
The denial code CO 197 can be problematic for healthcare providers, but understanding the common causes can reduce their occurrence in the future. Here’s a breakdown of some common scenarios and errors that lead to CO 197 denials:
Lack of Pre-authorization
This is the most frequent explanation for the condition. Some services call for prior authorization from the insurance company. When the healthcare provider fails to obtain this pre-authorization, the claim is denied under CO 197.
Incorrect Authorization
Even if the procedure of pre-authorization was tried, there could be some issues. Maybe the wrong code was entered or other information on the plan was incomplete. This can lead to a CO 197 denial as well. This is especially the case where the patient has filled out the application with false information.
Notification Issues
There are some insurance plans that ask for prior notification for certain procedures, even when they may not need pre-authorization. If the provider does not or cannot notify the insurer, the claim is denied under CO 197.
Experimental or Investigational Procedures
Insurance providers generally do not reimburse procedures considered to be experimental or investigational. If such a procedure is not documented to justify medical necessity and insurance coverage, then one is likely to see a CO 197 denial.
Failure to Follow Up
Typically, pre-authorization is not limited to submitting a pre-authorization request only. Failure to follow up on the status or assume approval results proves to be a reason for the CO 197 denial. All pre-authorization requests have to be recorded, and approvals have to be obtained before the procedures are embarked upon.
Failure to Follow Specific Guidelines
Sometimes insurance organizations have their own regulations that have to be fulfilled to get pre-authorization or pre-approval. Failure to adhere to these guidelines is likely to lead to the Code 197 denial.
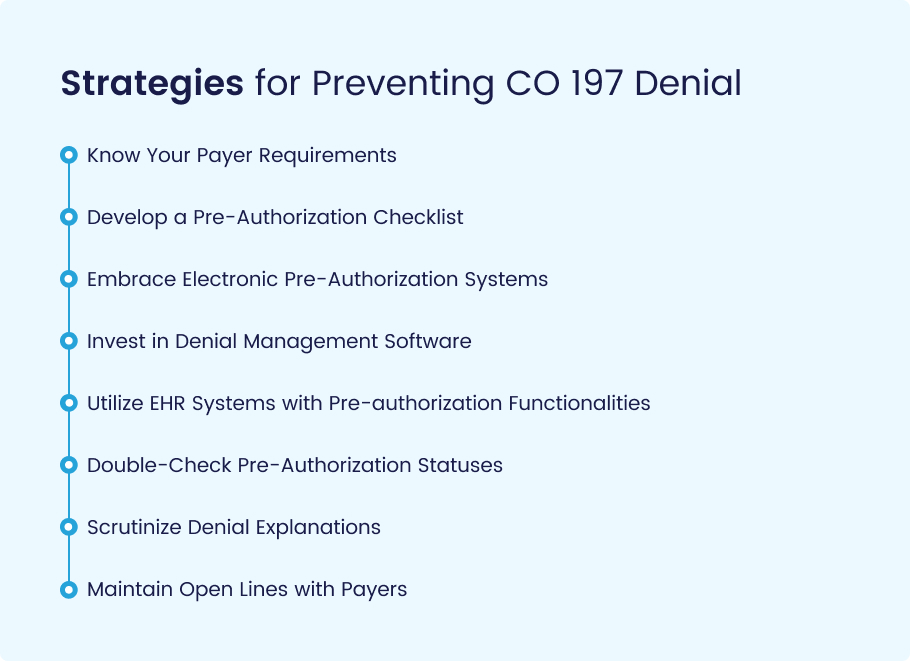
The CO 197 denial code can be destructive to the revenue cycle management if not well managed. But fear not! Here’s a targeted arsenal of strategies specifically designed to eliminate this authorization roadblock:
Know Your Payer Requirements
Ensure that you develop a list of all the pre-authorization requirements and keep an updated record of all the insurance companies you deal with. This list should state which services need preauthorization, notification, or certification and provide information on submission procedures and dates.
Develop a Pre-Authorization Checklist
Design a checklist that contains all the requirements that should be implemented in pre-authorization requests. This might include:
- Patient characteristics (demographics etc.)
- Listing of a particular service and procedure
- Contains specific clinical justification for any claim of medical necessity.
- Any other pertinent data that supports the test results, the physician notes, etc.
- Complete information about the patient and the provider, including their contact details.
Embrace Electronic Pre-Authorization Systems
Use EHR systems with pre-authorization features. This enables efficient submission of requests through electronic means and a constant check of the status of the requests to avoid issues like lost documents or missed timelines.
Invest in Denial Management Software
It may be helpful to use software that tracks denials, like CO 197, and alerts you to repeated patterns so you can explore possible underlying issues. This can assist you in identifying areas in which you require more practice.
Utilize EHR Systems with Pre-authorization Functionalities
Identify the EHR systems that have mechanisms for handling pre-authorization by submitting requests electronically and tracking their status. It also helps to minimize the chances of missed requests and/or deadlines.
Double-Check Pre-Authorization Statuses
Do not presume acceptance. Establish a culture of constant follow-up on pre-authorization requests and ensuring that approvals are sought before providing services.
Scrutinize Denial Explanations
If you have been given a CO 197 denial, review the EOB closely to understand the reason behind your denial. Determine which type of authorization was possibly not present (pre-authorization authorization, notification, or certification). It assists in identifying the root cause of the problem and where to focus the correction activities.
Maintain Open Lines with Payers
Ensure that the insurance companies you work with are well-established and reliable. It is advisable to visit their official website or other official channels to find out if there is any new change in their standard, in terms of pre-authorization, or in the way they communicate with you.
Implementing these strategies can successfully reduce the chances of CO 197 denials in your healthcare facility.
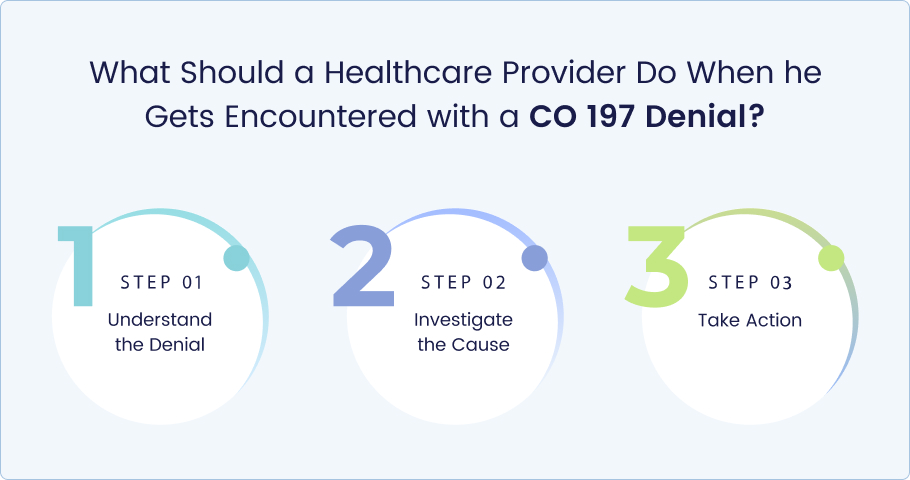
It is always a bit discouraging to encounter a CO 197 code denial, but here is what you can do. Following steps are a roadmap for navigating this situation and potentially recouping your reimbursement:
Step 1: Understand the Denial
Review the Explanation of Benefits (EOB): This letter from the insurance company will explain why the request has been turned down and will usually contain a particular number code (CO 197 in this instance). The EOB might also include comment codes that will provide additional explanation.
Identify the Missing Authorization: Review the EOB to determine what type of prior authorization was omitted (pre-authorization, notification, certification).
Step 2: Investigate the Cause
Internal Review: Check the records to find out whether an approval request was made earlier using the pre-authorization process. If so, there could be mistakes within the request that led to the denial of the particular request.
Communication Breakdown: In contemplating this idea, think about whether there has been a breakdown or a missed transmission of information between your practice and the insurance company. It is possible that the pre-authorized request was misplaced or not properly authorized.
Step 3: Take Action
Gather Supporting Documentation: If medical necessity was the issue, gather all pertinent patient information, lab work, and other physician-documented evidence that indicates the necessity of the service.
Appeal the Denial: It is always advisable to seek help from an insurance company, as the majority of them have provisions where an insured can appeal a denied claim. Submit a formal appeal along with the most recommended time frame and all the reasons as to why the service was relevant, as per the medical details you have collected.
Additional Options
Contact the payer: In certain situations, just a phone call to the insurance company’s medical billing section may offer a clear perspective on the controversy and possibly a solution.
Consider Retroactive Authorization: In certain cases, the insurer may allow you to seek retrospective approval for the service you seek to have done. This basically means asking for permission after the medical service has been provided, but with adequate supporting documentation of medical need.
By following the outlined procedures and being relentless, you can enhance your chances of successfully challenging the CO 197 denial and refilling the service offered.
Conclusion
In conclusion, the CO 197 denial code doesn’t have to be one that continually causes stress. It is crucial to know what causes denial, adopt an effective denial management system, and overturn your medical billing operations. The best practices include ensuring that accurate coding is done, completing all the pre-authorization requests, and learning about the insurance laws to avoid the denial of a pre-authorization request in the first place.
Implementing the strategies mentioned in your practice will decrease the possibility of CO 197 denials and help you receive timely reimbursements, or else outsource your medical billing and coding work to a reliable medical billing company.