Running a medical practice involves juggling numerous responsibilities—from patient care to managing billing processes. Among these tasks, charge entry in medical billing is one of the most crucial elements that directly impact your practice’s revenue cycle. But what exactly is charge entry, and why should healthcare providers prioritize it?
In this blog, we will guide you through the charge entry in medical billing, its role in the medical billing cycle, and how optimizing this step can enhance accuracy, reduce claim denials, and streamline your revenue cycle management (RCM). Along the way, we’ll highlight real-world scenarios and industry insights to help you fully grasp the value of charge entry.
Charge entry is the process of entering the charges (medical services or treatments) provided to a patient into a billing system. This step ensures that the services rendered are appropriately documented and billed to the insurance payer or the patient.
Charge entry closely links with medical coding and claims processing. For instance, the charges entered by a physician after seeing a patient will often be associated with the appropriate CPT (Current Procedural Terminology), ICD-10 (International Classification of Diseases), and HCPCS (Healthcare Common Procedure Coding System) codes that describe the services provided.
Charge entry is a crucial component of the claim submission process. Without accurate charge entry, the codes used during medical billing may not accurately align with the services provided. As a result, the insurance company will deny the claim.
Role in the Revenue Cycle
Charge entry in medical billing sits at the foundation of your entire revenue cycle. From charge capture to payment receipt, everything relies on accurate and timely charge entry. A small mistake in this step can lead to inaccurate billing, delayed payments, and even denials. This, in turn, disrupts the entire revenue cycle process.
On the other hand, if charges are entered accurately and data are maintained accordingly, this will keep the cash flow smooth and enhance the revenue cycle process.
Impact on Clean Claims Rate and Reimbursements
One of the main goals of the charge entry process is to ensure that clean claims are submitted. A clean claim is error-free, fully compliant with healthcare regulations, such as HIPAA, and contains all the necessary information. Accurate charge entry directly contributes to achieving a high clean claim submission rate, which improves reimbursement speeds and reduces administrative costs.
In fact, according to the American Academy of Professional Coders (AAPC), claims with errors can result in a delay of 20% or more in payment, and incorrect charges are the primary reason for claim denials.
Compliance and Audit Readiness
Charge entry also plays a crucial role in ensuring compliance with regulations such as HIPAA (Health Insurance Portability and Accountability Act) and CMS (Centers for Medicare & Medicaid Services). By ensuring that charges are entered accurately, practices are better prepared for audits, minimizing the risks of penalties.
Impact on Healthcare Providers
For healthcare providers, charge entry has a direct impact on revenue. Errors in this process can delay payment, reduce reimbursement amounts, and create additional administrative work to resolve issues.
Implications for Patients
When charge entry is accurate, it ensures that patients receive clear and correct billing statements, avoiding unexpected bills. Patient billing accuracy is crucial for maintaining trust and satisfaction. Incorrect charge entries can lead to patients being billed for services they never received or being charged incorrectly for their insurance coverage.
Role in Payer Relations
For payers (insurance companies), correct charge entry ensures that the claims they receive meet their requirements for reimbursement. Accurate claims reduce the likelihood of disputes, streamline the claims processing cycle, and foster positive relationships between providers and payers.
Importance of RCM Companies
RCM companies (Revenue Cycle Management) also rely on clean charge entries to optimize the billing and payment processes. Charge entry directly impacts their ability to maintain profitability for the practice, reduce operational costs, and ensure cash flow remains stable.
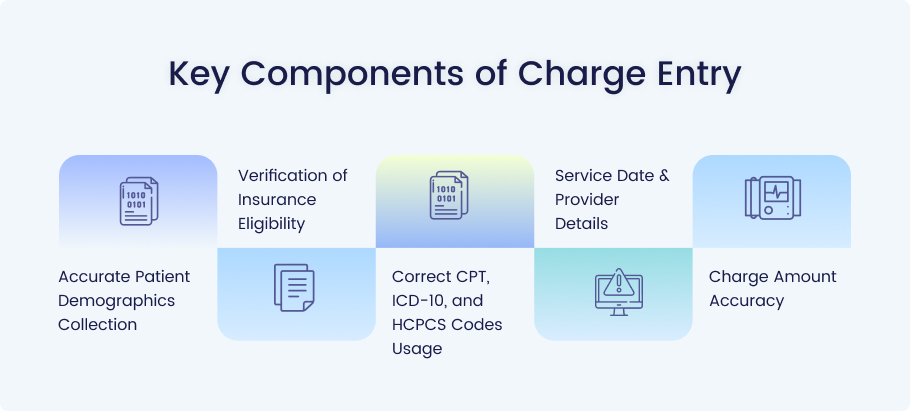
Accurate Patient Demographics Collection
It all starts with accurate patient demographics. This includes collecting basic yet essential information such as the patient’s name, date of birth (DOB), insurance details, and contact information. Without correct demographic data, the billing process can’t move forward.
Verification of Insurance Eligibility
Real-time insurance verification is another critical step. Verifying a patient’s insurance coverage at the time of service helps reduce the risk of denials. Many EHR/PM (Electronic Health Record/Practice Management) systems now integrate with insurance providers, ensuring up-to-date eligibility checks before charges are entered.
Correct CPT, ICD-10, and HCPCS Codes Usage
Correctly applying CPT, ICD-10, and HCPCS codes is a vital part of charge entry. Using incorrect codes or omitting necessary modifiers (such as modifier -25 for separate procedures) can result in claim rejections or inaccurate reimbursements.
Service Date & Provider Details
Accurate service date and provider details ensure that the charges match the services rendered. For example, billing a service on a date other than when it was provided can lead to complications, such as claim denials.
Charge Amount Accuracy
The charge amount must be accurately based on the practice’s fee schedule, payer agreements, or Usual, Customary, and Reasonable (UCR) rates. Incorrect amounts can trigger claim denials or delays.
Before charge entry even begins, there are a few essential pre-entry tasks:
- Appointment scheduling: Accurate scheduling ensures that the correct charges are generated.
- Insurance verification: Confirming insurance details beforehand helps prevent claim denials.
- Authorization confirmation: Many services require prior authorization, which must be validated before charges are entered.
Manual vs. Automated Charge Entry Tools
While some practices still perform charge entry manually, automated charge entry tools such as Kareo or AdvancedMD help eliminate errors and improve efficiency. Automation ensures that charges are entered quickly and accurately, and it can integrate with existing Electronic Health Records (EHR) systems to streamline workflows.
Workflow Best Practices
Best practices for efficient charge entry:
- Use a checklist to ensure all required fields are filled.
- Avoid duplicate entries by ensuring that charges are only entered once.
Internal Audits & Claim Scrubbing
After entering charges, conducting internal audits, and using claim scrubbing tools can help identify and correct potential errors before submission. These tools analyze submitted claims to ensure they meet payer requirements and reduce the chances of rejection.
Explanation of Benefits (EOB) Review
After submitting claims, reviewing the Explanation of Benefits (EOB) helps identify any issues that may arise. The EOB includes:
- Claim status
- Allowed amounts
- Deductibles/copays
- Denial reasons
Reviewing the EOB ensures that discrepancies are flagged and addressed promptly.
The providers and practices may encounter these challenges in the charge entry process in medical billing:
- Data entry errors: Typos or incorrectly entered data can delay payments and require rework.
- Incomplete patient information: Missing or incorrect details can result in denials.
- Frequent coding mistakes: Incorrect codes lead to claim rejections.
- Lack of standardization: Without uniform procedures, charge entry becomes prone to mistakes.
To maintain consistency, practices should:
- Develop Standard Operating Procedures (SOPs) for charge entry.
- Integrate charge capture tools within electronic health record (EHR) systems.
- Use checklists to ensure you don’t overlook essential details.
A well-trained billing team isn’t just important—it’s crucial for the smooth functioning of your medical practice’s revenue cycle. Charge entry may seem like a straightforward task, but many issues require expertise to ensure accuracy and efficiency.
1. Familiarity with Coding Guidelines
Accuracy is critical in medical billing and coding. The correct use of CPT (Current Procedural Terminology), ICD-10 (International Classification of Diseases), and HCPCS (Healthcare Common Procedure Coding System) codes ensures that your claims are compliant with payer requirements. When your billing team is trained on the latest coding guidelines, they can avoid common errors, such as:
- Upcoding: Charging for more expensive procedures than were performed.
- Downcoding: Charging for procedures at a lower rate than what was provided.
- Unbundling: Incorrectly breaking down services that should be billed as a package.
These coding errors can lead to claim denials, payment delays, or even audits. A trained team understands the importance of accurate coding and can apply these guidelines with confidence.
2. Error Handling Protocols
Even the best billing systems aren’t immune to human error. However, a well-prepared medical billing team is equipped with protocols to catch and correct mistakes before claims are submitted.
Some standard error-handling practices include:
- Claim Scrubbing: Before submission, claims should undergo a thorough review using automated tools that check for common coding and documentation errors.
- Denial Management: If a claim is denied, a trained team knows how to quickly identify the reason for the denial, gather any necessary documentation, and resubmit the claim accurately.
- Communication with Payers: A skilled team knows how to effectively communicate with payers to resolve issues such as underpayment, inaccurate coding, or missing documentation.
Error-handling protocols reduce the likelihood of costly rework, minimize claim rejections, and improve cash flow.
3. Productivity and Accuracy Metrics
A trained medical billing team not only focuses on accuracy but also on productivity. It’s about finding the right balance between speed and quality. Here are some key performance indicators (KPIs) that a billing team should track:
- Clean Claim Rate: The percentage of claims submitted without errors. A higher clean claim rate results in faster payments and fewer denials.
- Claim Denial Rate: The percentage of claims that are rejected. A well-trained team works to minimize this number by following best practices in charge entry and coding.
- Days in Accounts Receivable (A/R): This metric tracks the average number of days it takes for a practice to receive payment for services rendered. Efficient charge entry has a direct impact on this metric.
- First Pass Resolution Rate: The percentage of claims that get paid after the first submission. A trained team typically has a higher first-pass resolution rate, which reduces administrative overhead and improves overall efficiency.
Remember that training your team to track these metrics can have a direct impact on your bottom line by reducing delays and enhancing reimbursement rates.
Today, technology is not just a tool—it’s a game-changer for charge entry. The integration of AI-powered medical billing software has streamlined many aspects of the billing process, making it faster, more accurate, and far more efficient.
Real-Time Reporting and Analytics
AI-based billing systems enable practices to generate real-time reports on claims, payments, denials, and the status of accounts receivable (A/R) in seconds.
Real-time insights enable practices to:
- Identify issues early: For example, if a claim is flagged as potentially problematic, the billing team can address the issue before it’s submitted.
- Track KPIs: Practices can view metrics such as clean claim rates, denial rates, and payment trends in real-time, enabling faster decision-making and course corrections.
- Forecast cash flow: With up-to-date reports on claims and payments, practices can better predict when they will receive payment and make informed financial decisions.
Real-time reporting eliminates the guesswork from the billing process, thereby reducing the risk of financial surprises.
EHR Integration
The integration of billing software with Electronic Health Records (EHR) and Practice Management (PM) systems is a significant time-saver. When charge entry software is integrated with Electronic Health Records (EHRs), key patient data, including demographics, insurance details, and diagnoses, is automatically transferred into the billing system. This integration ensures:
- Reduced Data Entry Errors: By eliminating the need for manual data entry, the likelihood of errors, such as mistyped patient information or incorrect service dates, is significantly decreased.
- Improved Workflow: Billing teams can enter charges directly from the EHR, making it quicker and easier to submit accurate claims.
- Faster Payments: Integration
- ensures that all the required data for claims submission is accurate and up-to-date, improving the clean claim rate and leading to faster reimbursements.
Incorporating AI and EHR integrations into your charge entry process ensures that you aren’t wasting time on redundant tasks and reduces the chances of errors in charge capture.
Error Detection and Prevention
AI-powered software comes with built-in error detection tools. These tools can spot potential issues like:
- Incorrect coding (e.g., mismatched CPT and ICD-10 codes)
- Missing modifiers (e.g., -25 or 59)
- Incomplete patient information
By flagging these errors before submission, AI software helps your team avoid costly mistakes. The automation of routine tasks, such as verifying insurance eligibility or cross-checking coding accuracy, frees up your team to focus on more complex issues.
In addition to speed and accuracy, compliance and data security are paramount in charge entry. With healthcare becoming increasingly digitized, practices must adhere to strict regulations and ensure that patient data is kept secure.
1. HIPAA Compliance
The Health Insurance Portability and Accountability Act (HIPAA) sets the standard for protecting sensitive patient data. Medical billing teams need to:
- Maintain confidentiality: Charge entry systems should ensure that patient information is only accessible to authorized personnel.
- Encrypt data: Medical billing software must encrypt patient data both at rest and in transit to prevent unauthorized access.
- Monitor access: Access to charge entry data should be logged and monitored to detect any unauthorized attempts to access patient information.
Failure to comply with HIPAA can lead to significant financial penalties and damage to the practice’s reputation. A trained billing team ensures that all data handling is HIPAA-compliant, from charge entry to claim submission.
2. Data Security
Charge entry systems must include built-in security measures to prevent data breaches. These measures may include:
- Secure servers: Data should be stored on HIPAA-compliant servers with strong firewalls and encryption.
- Role-based access control (RBAC): Only those who need access to specific data (e.g., billing staff, insurance verifiers) should be able to view or modify it.
- Audit trails: The system should create logs that track all access and modifications to patient data, ensuring transparency and accountability.
With data breaches becoming more common in healthcare, maintaining strong security practices in charge entry is not just a regulatory requirement—it’s essential for protecting patient trust and safeguarding sensitive information.
Conclusion
Charge entry in medical billing is a vital component that impacts everything from preventing claim denials to managing the revenue cycle. By implementing best practices, utilizing the right tools, and ensuring proper training, you can significantly enhance your charge entry process, resulting in more accurate billing, faster reimbursements, and fewer claim denials.
Ready to optimize your charge entry process?
Contact Medheave to learn how we can support your medical practice with advanced billing solutions that improve efficiency and accuracy.