Anemia shows up a lot in patient charts. But coding it correctly isn’t always simple. One wrong character can lead to denials, delays, or underpayment.
So, as a healthcare provider, you must be aware of the ins and outs of anemia coding.
Because the revenue is the bottom line, and wrong anemia codes can cause revenue loss.
Let’s walk through what coders and healthcare providers need to know about Anemia ICD-10 codes.
What Is the ICD-10 Code for Anemia?
Anemia happens when the body doesn’t have enough healthy red blood cells to carry oxygen.
It’s common in people with chronic illnesses, nutritional deficiencies, or those undergoing treatment like chemotherapy.
In ICD-10 terms, anemia falls under Chapter D50–D64. It includes several subtypes—each one with its own codes and documentation needs.
Why Correct Anemia Coding Matters
When anemia is under-coded or misclassified, it leads to:
- Claim denials
- Lower reimbursement
- Lost revenue
Many providers default to the generic code D64.9 (ICD-10 code for anemia unspecified).
But payers are watching that closely.
That unspecified anemia ICD-10 code doesn’t tell them why the patient is anemic, which is often critical for payment collection and care quality.
Because, the insurance payer rejects the claim.
At the end of the day, this all leads to lower reimbursements and revenue loss.
ICD-10-CM Overview of Anemia Codes
When talking about anemia coding, as a healthcare provider, you must know where these codes live in the ICD-10 system.
Consider ICD-10 as a big library of medical codes.
And you need to identify the anemia ICD-10 codes.
Each disease has its own section.
Anemia codes are found in Chapter 3 of the ICD-10-CM manual on CMS. You can also get ICD-10 Codes for anemia on AAPC’s CPT Codes Lookup Tool called Codify.
However, the CMS chapter 3 covers “Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism.”
That’s a mouthful. But it’s important to know where to look.
The specific codes for anemia range from D50 to D64.
Centers for Medicare & Medicaid Services (CMS) classifies anemia based on its cause.
The cause determines the code. Simple enough?
But here’s where it gets tricky.
Many providers use the unspecified code D64.9 when they can’t determine the exact type.
This might seem like an easy solution. But it’s actually quite risky.
Let’s see why D64.9 is problematic.
Payers like Medicare look closely at unspecified codes. They want to know the specific type of anemia. They want to see that you’ve done the work to find the cause.
Using D64.9 without proper documentation can lead to claim denials. It can also trigger audits. And it definitely doesn’t help with appropriate patient care documentation.
Here’s what you need to know about the anemia code categories:
- The D50-D53 codes cover anemias due to nutritional deficiencies. This includes iron deficiency, vitamin B12 deficiency, and folate deficiency.
- The D55-D59 codes cover hemolytic anemias. These occur when red blood cells are destroyed faster than they can be made.
- The D57 codes cover sickle cell disorders.
- The D60-D61 codes cover aplastic and other bone marrow failure syndromes.
- The D63 codes cover anemia in chronic diseases.
- The D64 codes cover other and unspecified anemias.
Understanding these categories is the first step to accurate coding.
But we’ll dig deeper into each one as we go along.
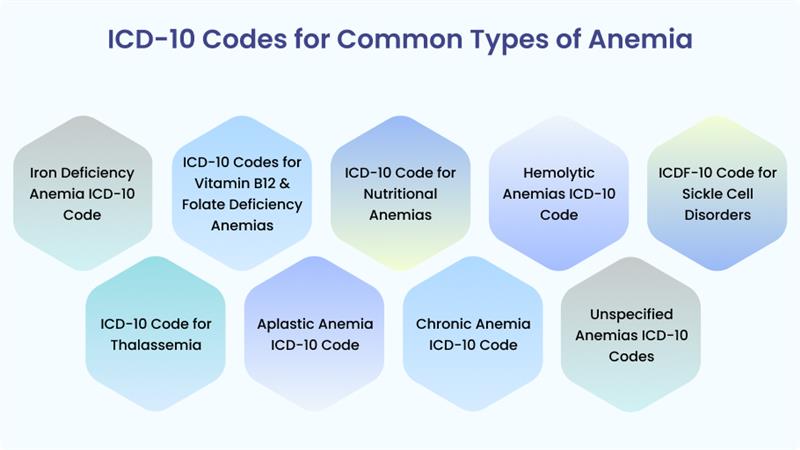
ICD-10 Codes for Common Types of Anemia
Anemia isn’t just one condition. It’s a group of conditions with different causes. Each type needs its own specific code.
Let’s walk through the most common types of anemia you’ll see in your practice.
So, you must know how to code them and what documentation you need.
Iron Deficiency Anemia ICD-10 Code
Iron deficiency anemia is the most common type of anemia worldwide.
It happens when your body doesn’t have enough iron to make hemoglobin. Without enough iron, a patient can’t carry oxygen effectively.
For coding iron deficiency anemia, you’ll use codes from the D50 category.
But it’s not just one code.
Here are Iron deficiency anemia ICD-10 codes depending on the specific cause:
- D50.0: Iron deficiency anemia secondary to blood loss (chronic)
- D50.1: Sideropenic dysphagia
- D50.8: Other iron deficiency anemias
- D50.9: Iron deficiency anemia, unspecified
When documenting iron deficiency anemia, be specific about the cause.
- Is it due to chronic blood loss? Is it dietary?
- Is it related to a condition like celiac disease?
The more specific you can be, the better your coding will be.
Remember to link the anemia to the underlying cause in your documentation.
ICD-10 Codes for Vitamin B12 & Folate Deficiency Anemias
These anemias occur when your body lacks vitamin B12 or folate.
Both are essential for making healthy red blood cells. Without them, red blood cells can’t mature properly.
They end up being large and fragile. This condition is called megaloblastic anemia.
The ICD-10 codes for B12 deficiency anemia from the D51 category include:
- D51.0: Pernicious anemia
- D51.1: Other vitamin B12 deficiency anemias
- D51.2: Transcobalamin II deficiency
- D51.3: Other dietary vitamin B12 deficiency anemia
- D51.8: Other vitamin B12 deficiency anemias
- D51.9: Vitamin B12 deficiency anemia, unspecified
For folate deficiency anemia, you’ll use codes from the D52 category:
- D52.0: Dietary folate deficiency anemia
- D52.1: Drug-induced folate deficiency anemia
- D52.8: Other folate deficiency anemias
- D52.9: Folate deficiency anemia, unspecified
When documenting these conditions, note the cause.
- Is it dietary?
- Is it due to malabsorption?
- Is it drug-induced?
Also, document any treatments the patient is receiving, such as B12 injections or folate supplements.
ICD-10 Code for Nutritional Anemias
Nutritional anemias go beyond just iron, B12, and folate deficiencies. They include anemias caused by other dietary deficiencies.
These are less common but still important to recognize.
ICD-10 Codes in this category include:
- D53.0: Protein deficiency anemia
- D53.1: Other megaloblastic anemias, not elsewhere classified
- D53.2: Scorbatic anemia
- D53.8: Other specified nutritional anemias
- D53.9: Nutritional anemia, unspecified
When documenting nutritional anemias, be specific about the deficiency.
Note any dietary restrictions or conditions that might contribute to the deficiency. Also, document any nutritional supplements the patient is taking.
Hemolytic Anemias ICD-10 Code
Hemolytic anemias occur when red blood cells are destroyed faster than they can be made.
This destruction is called hemolysis.
It can happen inside the blood vessels (intravascular) or outside the blood vessels (extravascular).
Hemolytic anemias can be inherited or acquired.
The codes for hemolytic anemias include:
- D55: Anemias due to enzyme disorders
- D56: Thalassemia
- D57: Sickle-cell disorders
- D58: Other hereditary hemolytic anemias
- D59: Acquired hemolytic anemia
Each of these categories has specific subcodes. For example, D57 includes codes for different types of sickle cell disorders.
D59 includes codes for autoimmune hemolytic anemias, drug-induced hemolytic anemias, and other acquired hemolytic anemias.
When documenting hemolytic anemias, note the cause if known.
- Is it hereditary?
- Is it autoimmune? Is it drug-induced?
Also, document any signs of hemolysis, such as jaundice, dark urine, or an enlarged spleen.
ICDF-10 Code for Sickle Cell Disorders
Sickle cell disease is a group of inherited red blood cell disorders. The red blood cells become hard and sticky and look like a C-shaped farm tool called a “sickle.”
These cells die early, causing a shortage of red blood cells.
They can also get stuck and block blood flow, causing pain and other serious problems.
Codes for sickle cell disorders include:
- D57.00: Hb-SS disease with crisis, unspecified
- D57.01: Hb-SS disease without crisis
- D57.1: Sickle-cell/Hb-C disease
- D57.2: Sickle-cell/beta-thalassemia
- D57.3: Sickle-cell trait
- D57.4: Sickle-cell disease NOS
- D57.8: Other sickle-cell disorders
When documenting sickle cell disorders, be specific about the type. Note if the patient is in crisis.
Document any complications, such as pain, infections, or organ damage.
Also, document any treatments, such as hydroxyurea or blood transfusions.
ICD-10 Code for Thalassemia
Thalassemia is another inherited blood disorder.
It causes the body to make less hemoglobin than normal. Hemoglobin is the protein in red blood cells that carries oxygen.
Thalassemia can cause anemia and other health problems. That’s why ICD-10 codes assigned in various clinical conditions
ICD-10 Codes for thalassemia include:
- D56.0: Alpha thalassemia
- D56.1: Beta thalassemia
- D56.2: Delta-beta thalassemia
- D56.3: Thalassemia trait
- D56.4: Thalassemia intermedia
- D56.5: Hemoglobin E-beta-thalassemia
- D56.8: Other thalassemias
- D56.9: Thalassemia, unspecified
When documenting thalassemia, be specific about the type. Note the severity.
Document any complications, such as iron overload from frequent transfusions.
Also, document any treatments, such as blood transfusions or chelation therapy.
Aplastic Anemia ICD-10 Code
Aplastic anemia is a rare but serious condition.
It occurs when the bone marrow fails to produce enough blood cells.
This can be due to bone marrow failure. It can be inherited or acquired.
Acquired causes include autoimmune disorders, infections, and exposure to certain drugs or chemicals.
ICD-10 codes for aplastic anemia include:
- D60.0: Chronic acquired pure red cell aplasia
- D60.1: Transient erythroblastopenia of childhood
- D60.8: Other specified acquired pure red cell aplasias
- D60.9: Acquired pure red cell aplasia, unspecified
- D61.0: Constitutional aplastic anemia
- D61.1: Drug-induced aplastic anemia
- D61.2: Aplastic anemia due to other external agents
- D61.3: Idiopathic aplastic anemia
- D61.8: Other specified aplastic anemias
- D61.9: Aplastic anemia, unspecified
When documenting aplastic anemia, note the cause if known.
- Is it congenital?
- Is it drug-induced?
- Is it due to an infection?
Document any treatments, such as immunosuppressive therapy or bone marrow transplant. Also, document any complications, such as infections or bleeding.
Chronic Anemia ICD-10 Code
Anemia in chronic disease is also called anemia of chronic inflammation.
It occurs in people with chronic infections, autoimmune disorders, or chronic kidney disease.
The chronic inflammation affects the body’s ability to use iron to make red blood cells.
Codes for anemia in chronic disease include:
- D63.0: Anemia in neoplastic disease
- D63.1: Anemia in chronic kidney disease (CKD)
- D63.8: Anemia in other chronic diseases classified elsewhere
When documenting anemia in chronic disease, link the anemia to the underlying condition.
For example, document “anemia due to chronic kidney disease” rather than just “anemia” and “chronic kidney disease” separately.
This ensures proper code sequencing and helps prevent denials.
Other & Unspecified Anemias ICD-10 Codes
This category includes anemias that don’t fit into the other categories.
It also includes unspecified anemias.
While unspecified codes should be avoided, when possible, sometimes they’re necessary when the cause can’t be determined.
Codes in this category include:
- D64.0: Hereditary sideroblastic anemia
- D64.1: Secondary sideroblastic anemia due to disease
- D64.2: Secondary sideroblastic anemia due to drugs and toxins
- D64.3: Other sideroblastic anemias
- D64.4: Congenital dyserythropoietic anemia
- D64.8: Other specified anemias
- D64.9: Anemia, unspecified
When documenting anemias in this category, be as specific as possible.
Avoid using D64.9 unless necessary.
If you must use an unspecified code, document your efforts to determine the cause.
This can help if the claim is reviewed or audited.
ICD-10 Anemia Coding Guidelines & Documentation Tips
Now that we’ve covered the different types of anemia and their codes, let’s talk about how to code them correctly.
Remember that medical coding isn’t just about picking the right code. It’s about following guidelines and documenting properly.
Let’s dive into some key ICD-10 Anemia guidelines and tips.
- Linking anemia to its underlying: You must link anemia to underlying correctly. According to ICD-10-CM guidelines, when a patient has both anemia and a condition that can cause anemia, you should link them. For example, if a patient has chronic kidney disease and anemia due to the CKD, you should code both the ICD-10 codes for anemia in chronic kidney disease (CKD) and D63.1 (anemia in chronic kidney disease). This shows the relationship between the two conditions. And this helps insurance payers understand the exact procedure and its code.
- Code sequencing: Code sequencing is also important for giving a hint to the payer for the accuracy in procedure/service. In general, the underlying condition should be coded first, followed by the anemia. For example, for a patient with anemia due to CKD, you would code the chronic kidney disease (CKD) first, then D63.1. This follows the ICD-10-CM guidelines for coding “due to” conditions.
- Using lab results: Lab results can support your coding. Complete blood count (CBC) results showing low hemoglobin or hematocrit can support an anemia diagnosis. Iron studies can support iron deficiency anemia. Vitamin B12 and folate levels can support deficiency anemias. Including these lab results in your documentation can strengthen your coding and help prevent denials.
- Avoiding unspecified codes: Avoiding unspecified codes is another key guideline. Unspecified codes like D64.9 should only be used when you can’t determine a more specific code. Payers often scrutinize unspecified codes. They may deny claims or request additional documentation. Always try to find the most specific code possible.
Here are some additional documentation tips:
- Document the type of anemia clearly in the assessment or impression section.
- Note the cause of the anemia if known.
- Include relevant lab results and their interpretation.
- Document any treatments provided for the anemia.
- Link the anemia to any underlying conditions.
- Document any symptoms the patient is experiencing due to the anemia.
- If using an unspecified code, document why a more specific code couldn’t be used.
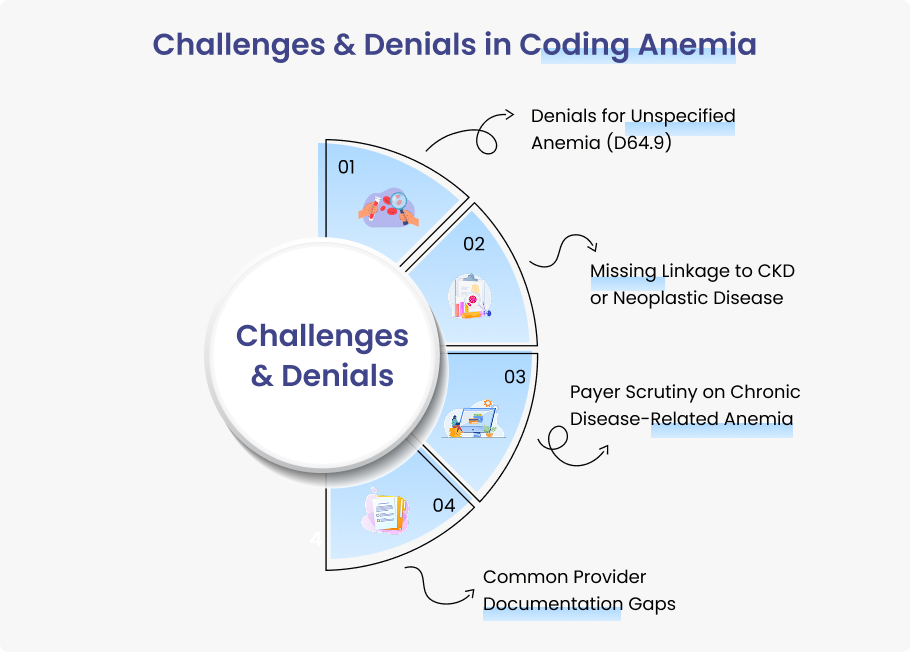
Challenges & Denials in Coding Anemia
Coding anemia isn’t always straightforward. Many challenges can lead to denials.
Here are some common challenges and some precautionary measures for providers to handle these challenges.
Denials for Unspecified Anemia (D64.9)
One of the most common reasons for denials is the use of unspecified codes like D64.9. Payers want to see specific codes.
They want to know the type and cause of the anemia. When you use an unspecified code, it raises red flags. Payers may think you haven’t done a thorough evaluation.
Insurance companies may deny the claim or request additional documentation.
To avoid denials for unspecified anemia:
- Always try to find the most specific code possible.
- Use D64.9 and document your efforts to determine the cause.
- Note any tests you ordered and their results.
- Explain why a more specific diagnosis couldn’t be made.
Missing Linkage to CKD or Neoplastic Disease
Another common challenge is failing to link anemia to underlying conditions like CKD or neoplastic disease.
Payers want to see this linkage. They want to know that the anemia is due to the underlying condition, not just a separate finding.
To avoid this issue:
- Always document the relationship between the anemia and the underlying condition.
- Use phrases like “anemia due to” or “anemia associated with.”
- Ensure the link is clear and ensures proper code sequencing.
Payer Scrutiny on Chronic Disease-Related Anemia
Payers often scrutinize claims for chronic disease-related anemia.
They want to make sure the anemia is truly related to the chronic disease.
They may request additional documentation or even deny the claim if they’re not convinced.
Remember, the more thorough your documentation, the less likely you are to face denials.
- Document anemia procedures, codes uses and patient details correctly.
- Note the chronic disease and how it’s causing the anemia.
- Include relevant lab results. Document any treatments provided for both conditions.
Common Provider Documentation Gaps
Documentation gaps are another common challenge. Providers may not document the type or cause of anemia clearly. They may not link the anemia to underlying conditions. They may not include relevant lab results. These gaps can lead to coding errors and denials.
To avoid documentation gaps:
- Use templates that prompt for all necessary information.
- Train providers on the importance of thorough documentation.
- Have coders query providers when documentation is unclear or incomplete.
Anemia Coding and Reimbursement Impact
Proper anemia coding doesn’t just prevent denials. It also impacts reimbursement.
See how incorrect coding can affect your bottom line.
How does incorrect anemia coding impact HCC risk adjustment?
Incorrect anemia coding can impact HCC (Hierarchical Condition Category) risk adjustment.
HCCs are used by Medicare and other payers to predict healthcare costs. Certain types of anemia can increase a patient’s risk score.
This affects reimbursement under value-based payment models. If you code incorrectly, you may not get the reimbursement you deserve.
Medicare & commercial payer considerations
Medicare and commercial payers have specific policies for anemia coding.
They may have different requirements for documentation and code selection. They may also have different reimbursement rates for various types of anemia.
Understanding these policies is crucial for proper reimbursement.
Here’s a case example. Consider a patient with chronic kidney disease and anemia due to the CKD.
If you code the CKD and D64.9 (anemia, unspecified), you may not get the same reimbursement as if you code the CKD and D63.1 (anemia in chronic kidney disease).
The latter shows the relationship between the two conditions and may qualify for higher reimbursement.
Another example is a patient with cancer and anemia due to chemotherapy.
Coding the cancer, the chemotherapy, and D64.0 (anemia secondary to antineoplastic chemotherapy) can result in higher reimbursement than coding the tumor, chemotherapy, and D64.9 (anemia, unspecified).
Best Practices for Coders & Providers
To ensure accurate anemia coding and prevent denials, follow these best practices:
Standardize documentation templates
- Use templates that prompt providers to document the type and cause of anemia.
- Include fields for linking anemia to underlying conditions.
- Include fields for relevant lab results. Standardized templates ensure all necessary information is captured.
Conduct periodic coder-provider training
- Train providers on the importance of thorough documentation.
- Train coders on the nuances of anemia coding.
- Bring them together to discuss common issues and solutions.
Audit claims with anemia codes
- Regularly review claims with anemia codes to identify patterns of errors or denials.
- Use these audits to identify areas for improvement.
- Share the findings with providers and coders to prevent future issues.
Consider working with expert billing partners
Medical billing and coding can be complex, especially for conditions like anemia.
- Partner with billing experts like Medheave to ensure accurate coding and maximum reimbursement.
- Establish relationships with other providers to navigate the complexities of anemia coding.
Conclusion
Anemia coding is complex. But it’s crucial for accurate reimbursement and proper patient care.
By understanding the different types of anemia and their codes, following anemia medical coding guidelines, and documenting thoroughly, you can prevent denials and ensure maximum reimbursement.
Remember to be as specific as possible when coding anemia unspecified vs specified.
Avoid unspecified codes unless necessary. Link anemia to underlying conditions. Document thoroughly.
And stay up to date with anemia medical coding guidelines and payer policies.
Need help coding complex anemia cases?
Contact Medheave’s certified coders to maximize reimbursement and reduce denials.
FAQs
What is the ICD-10 code for unspecified anemia?
The ICD-10 code for unspecified anemia is D64.9. This code should only be used when you can’t determine a more specific type of anemia. Payers often scrutinize this code, so it’s best to use a more specific code when possible.
How do you code anemia due to chronic kidney disease?
Anemia due to chronic kidney disease is coded as D63.1. You should also code the chronic kidney disease itself. The CKD code should be listed first, followed by D63.1. This shows the relationship between the two conditions.
What ICD-10 codes for iron deficiency anemia?
Iron deficiency anemia is coded using codes from the D50 category. The specific code depends on the cause. D50.9 is used for iron deficiency anemia, unspecified. D50.0 is used for iron deficiency anemia secondary to blood loss. D50.8 is used for other iron deficiency anemias.
Why is D64.9 considered high risk for denials?
D64.9 is considered high risk for denials because it’s an unspecified code. Patients want to see specific codes that show the type and cause of the anemia. When you use D64.9, it suggests that you haven’t done a thorough evaluation or that your documentation is incomplete. Payers may deny the claim or request additional documentation.
How can providers reduce anemia coding errors?
Providers can reduce anemia coding errors by documenting thoroughly. They should specify the type and cause of anemia. They should link anemia to any underlying conditions. They should include relevant lab results. They should also work closely with coders to ensure accurate code selection. Regular training and audits can also help reduce errors.