Patient, doctor, or provider, and billing services are three different entities in a medical claim. A claim’s entity code rejection occurs when one or all of the codes added to the claim are invalid. There are many reasons for this, including that a code is missing, expired, or inaccurate.
Similarly, a patient’s ID code can be the reason if it is outdated. An incorrect national provider identifier (NPI) number is also a common cause of claim rejection. A professional medical coding service can take remedial actions, such as editing the codes or updating them, and resubmit for reimbursement.
In most cases, a wrong billing NPI (the equivalent of Box 33 on the CMS-1500) or an incorrect tax ID given in Box 25 on the claim leads to a code rejection error when submitting a medical claim. In this blog, we will discuss all the reasons that play a pivotal role in claim denials caused by entity codes. Thus, we will also be presenting solutions to each problem, so your coding team remains on top of things. Without further ado, let’s discuss it in detail.
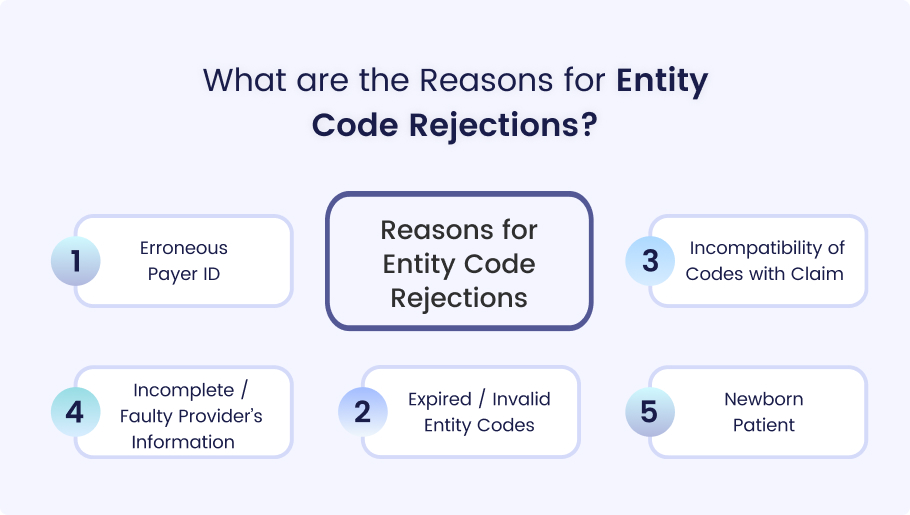
There can be many reasons that cause rejection from payers. By accurately identifying these reasons, medical billers can file claims that are reimbursed quickly. Typically, the reasons surrounding this query revolve around the following causes:
- Erroneous Payer ID
- Expired / Invalid Entity Codes
- Incompatibility of Codes With Claim
- Incomplete / Faulty Insurance Provider Information
- Newborn Patient
Let’s discuss these points in a systematic and detailed way so a proper rectification can be presented accordingly.
1. Erroneous Payer ID
Payer ID is a five-digit alphanumeric or numeric code that is unique. Every insurance company has its own code that helps identify them. When a medical biller adds an incorrect payer ID, this leads to autonomic rejection. As these claims are submitted electronically, the insurance company’s software is unable to recognize them, therefore directly leading to claim rejection.
2. Expired / Invalid Entity Codes
The second mistake that has the potential to lead to an entity code rejection is the use of expired or invalid codes. Medical codes are changed after the introduction of new specialties and procedures. Therefore, insurance claim codes are evolving rapidly. The use of older or invalid codes is detected as unrecognized, thus affecting the reimbursement process.
3. Incompatibility of Codes with Claim
Compatibility between codes and their subsequent relevance to claim data is of prime importance. The input code must translate into the procedure or service rendered. Any mismatch results in interpretation errors, further fueling the delays. These mistakes are very common among untrained staff and also due to the use of manual billing processes.
4. Incomplete / Faulty Provider’s Information
The provider is the one who is giving the best medical care to the patient(s). NPI (national provider identifier) is a unique ten-digit code. Every medical practitioner is given a unique code that helps insurance companies identify them.
Any mistake in accurately adding a physician’s NPI results in a discrepancy and thus results in entity code rejection. Accurate NPI helps create a correlation between claim and provider, enhancing reimbursement chances by many folds.
5. Newborn Patient
In gynecology departments, many claim issues related to deliveries arise on a regular basis. Newborn babies are entitled to their parent(s) insurance plan. The problem becomes apparent when the details of a new-born baby are not added or late added to the plan. Hastily sending these claims results in immediate rejection since that child’s information is not available to the insurance provider.
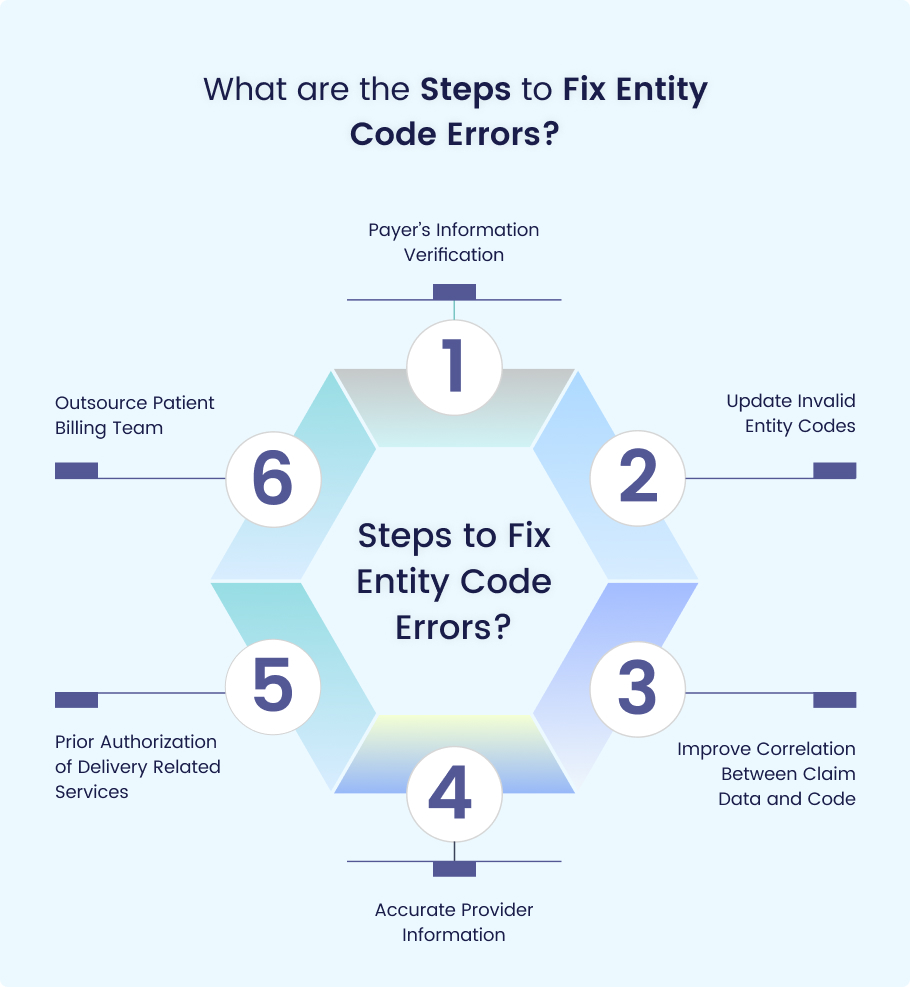
Just like the problems we have mentioned, as promised, the solutions will also be given. These remedial actions, once taken by a healthcare provider(s), can rectify many billing issues appropriately. After taking the following steps, hospitals, clinics, and private practices can easily avoid entity errors in patient claims.
1. Payer’s Information Verification
The big step in resolving these issues starts with verifying the payer’s information. A healthcare facility’s medical biller has a responsibility to double-check all the details pertaining to the insurance company.
Paying attention to this step can have beneficial outcomes because an accurate payer’s ID facilitates reimbursement. Following this process helps in avoiding resubmissions and future editing requirements.
2. Update Invalid Entity Codes
The second step the patient billing and coding department can take is updating their current inventory of codes. All invalid codes can be discarded, and updated coding guidelines for new medical specialties should be added. This act will permit coding professionals to use current codes, hence further enhancing your claim’s acceptance status.
3. Improve Correlation Between Claim Data and Code
This third step is the most relevant but is overlooked by the billing team. Healthcare establishments can integrate a dedicated quality control system. Although this one step is expensive and may cost more, it will ensure a match between codes and claims. The claim scrubbing team will look at every claim before it is submitted, so the providers can expect a greater outcome..
4. Accurate Provider Information
The fourth remedial action is adding accurate provider or physician’s information. Accurate mention of the NPI (national provider identifier), a ten-digit unique code assigned to each physician, helps propel a medical claim forward.
Medical coders can add a complete and authentic NPI in box 33a in the cms-1500 form. Doing so will result in a perfect match between the services provided by a physician and the claim submitted on behalf of those services.
5. Prior Authorization of Delivery Related Services
Claim-related issues due to the delivery of new-born babies can be rectified by obtaining prior authorization from the payer’s health plan. Medical billing teams can avoid delays and costly rejections with preauthorization. They can contact insurance companies and ask for approval on behalf of a patient’s new-born baby induction in the plan.
After receiving this approval, any medical service provided to the mother can be expedited for reimbursement quickly.
6. Outsource Patient Billing Team
Even after taking all five steps, healthcare facilities and providers still bear the cost of entity code rejections. The main reasons are identified as overburdening administrative staff and burnout. The best solution that can be applied, irrespective of the size of the specialty, is outsourcing billing staff. A third party clearinghouse allows efficiency and higher capability in processing these cases smoothly.
Additionally, professional patient billing companies can ensure greater transparency and the use of appropriate codes. Secondly, the coding and billing teams of these organizations are trained and skilled in their respective fields. This leaves providers less burdened with the tedious job of arranging training for new staff and refresher courses for older ones.
The Sum Up
The solution pertaining to entity code rejection lies in claims free of mistakes. Any medical claim that avoids these errors is accepted and reimbursed without delay. It is a well-established fact that common mistakes revolve around incorrect provider IDs, expired or invalid entity codes, mismatched claim data with codes, incomplete insurance provider’s information, and the possibility of the patient being a newborn.
To conclude, outsourcing a reputed and professional medical billing company like Medheave offers best options. Hiring our billing and coding team helps providers get the maximum amount of claims submitted without the fear of rejection. It is up to providers to optimize their revenue cycle management by either outsourcing or train their in-house team from professionals.